You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Glossary:
angioplasty—alteration of the blood vessel either surgically or by dilating a balloon in the vessel.
apicoectomy—excision of the root of a tooth.
arrhythmias—irregular heart rhythms.
asymptomatic—without symptoms.
atrophic—decreased in size.
auscultation—the process of listening for sounds in the body.
autoimmune—a disease produced when the body’s normal tolerance of its own antigenic markers on cells disappears.
bacteremia—bacteria in the blood.
basement membrane—level in tissues where generation of new cells occurs.
bradycardia—slow heart rate characterized by a pulse rate below 60 beats per minute.
bronchiectasis—chronic dilation of the bronchus or bronchi, with a secondary infection that usually involves the lower portion of the lung.
cannula—a tube or sheath enclosing a sharp surgical instrument, typically used with intravenous administration.
capnograph—a machine that records the carbon dioxide level in expired air in the mechanically ventilated individual.
cardiomyopathy—disease of the myocardium caused by primary disease of the heart muscle.
cheilosis—inflammation of the lip.
chorda tendinae—the tendons that hold the free edges of the atrioventricular valves to the papillary muscles preventing inversion of these valves during ventricular systole.
coagulation—clotting.
congenital—present at birth.
deficit—deficiency.
demethylation—removal of a methyl group (CH3) during chemical reactions.
desaturated blood—blood with lowered levels of oxygen.
DNA—nucleic acid containing genetic information.
dysrhythmias—abnormal heart rhythms.
ecchymosis—bruising of the tissue.
edema—swelling as a result of excessive tissue fluid.
epitaxis—nosebleed.
extracellular—outside the cell.
fibrin—a protein formed by the action of thrombin on fibrinogen; important in blood clots.
glossitis—inflammation of the tongue.
glucose—blood sugar.
hemophilia—a hereditary disease characterized by abnormal blood clotting.
hemostasis—the stoppage of bleeding.
hyperthyroidism—overproduction of thyroxine by the thyroid gland.
hypertrophic—an increase in size.
hypothalamus—portion of the brain that controls the release of hormones.
hypothyroidism—underproduction of thyroxine by the thyroid gland.
hypoxia—oxygen deficiency.
immunosupression—compromised immune system.
intravascular—within blood vessels.
intravenous—within or into a vein.
limbic system—a group of brain structures influencing the endocrine and autonomic motor systems.
lingula—a bony projection that forms the medial boundary of the mandibular foramen.
morbidity—state of being diseased.
myocardial infarction—a heart attack.
neuroma—any type of tumor composed of nerve cells.
orthopnea—breathing difficulty in any position but upright.
parenterally—denotes a medication route of administration other than by mouth; intravenous, subcutaneous, intramuscular, or mucosal.
petechiae—small bruises that can appear in the oral cavity.
perioperative—before, during, and after a surgical treatment or procedure.
proviral—before the viral stage.
pterygoid—muscle in the cheek that attaches to the mylohyoid bone.
pulse-oximeter—a device that records the pulse and oxygen concentration in the arterial blood.
ramus—a branching of a structure, as seen in the mandible.
RNA—the nucleic acid that controls protein synthesis in all living cells and takes the place of DNA in certain viruses.
saturated blood—blood full of oxygen.
sialogues—products that promote salivary flow.
sialoliths—salivary stones.
tachycardia—an abnormally high heart rate, usually greater than 100 beats per minute in adults.
thalamus—the portion of the brain responsible for all sensory stimuli with the exception of the olfactory sensations.
thrombin—an enzyme formed in shed blood from prothrombin, which converts fibrinogen into fibrin; the basis of the blood clot.
thrombocytopenia—an abnormal decrease in the amount of blood platelets.
trigone—triangular space in the retromolar area.
vasoconstrictors—drugs that narrow the blood vessels.
Von Willebrand disease—a congenital bleeding disorder caused by a deficiency in the coagulation actor VIII.
ROLE OF THE OMS DENTAL ASSISTANT
The role of the dental assistant in an oral and maxillofacial surgery setting can vary. Oral surgery assistants may be registered or certified dental assistants who have received additional experience in an oral surgery setting. Some assistants take an American Association of Oral and Maxillofacial Surgeons home study course, which allows them to sit for an examination for certification as an oral surgery anesthesia assistant. Dental assistants in an oral surgery setting must be well-trained in cardiopulmonary resuscitation and medical emergency procedures because many of their clients are referred to the specialty practice due to poor health or as victims of trauma.
Intraoral Responsibilities
The dental assistant is responsible for preparing all of the armamentarium and medications that will be used in the administration of anesthesia and in performing the surgical procedure. During the actual procedure, the assistant should maintain a clear working field for the dentist or surgeon through the use of evacuation and retraction. The assistant may also be responsible for observing and monitoring the client’s vital signs to ensure client safety during the surgery and anesthesia. Some states may allow the assistant to remove sutures or pack and remove socket medicament.
Client Management Responsibilities
The surgery dental assistant plays a major role in client management. Client management duties can range from reassuring the client prior to surgery to providing pre- and postoperative instructions. The surgery assistant may also make follow-up calls to the client later in the day to reaffirm client understanding of the instructions given, answer questions, or discuss any complications that may have arisen.
Infection Control Responsibilities
As with any dental office, the oral and maxillofacial surgery practice must use standard precautions in instrument preparation, sterilization, and medical waste management. Because oral surgery involves the invasion of hard and soft tissues, proper sterilization is imperative.
CLIENT HEALTH ASSESSMENT AND VITAL SIGNS
A medical assessment must be taken for every client who is to receive surgical treatment. A written, patient-completed medical history questionnaire is a legal necessity. The extent and detail of the medical history are somewhat dependent upon the surgeon’s personal preference and the type of surgical services to be rendered. However, the surgeon must be prepared to interpret how a medical problem will alter a client’s response to dental surgery and anesthetic agents. The health assessment may have to be abbreviated for some emergency procedures, but it must be completed before the end of the initial visit. Certain conditions such as language barriers, pain, and anxiety may affect the medical assessment interview and may need to be attended to before completion of the medical assessment.
OMS Management of Clients with Underlying Medical Conditions
Cardiovascular Diseases
Cardiovascular disease affects many dental clients. The disease may be hereditary or a result of lifestyle choices. It is important to postpone elective treatment in those clients who have had a cardiac episode within the last 6 months. If the procedure is considered an emergency and cannot be postponed, consultation with the client’s cardiologist is of utmost importance.
Ischemic heart disease is defined as a local and temporary deficiency in the blood supply to a particular region of the body, most commonly the heart. There are several factors that may lead to decreased circulation in the heart. Recommendations for clients with poorly controlled ischemic heart disease, labile cardiac rhythms, or potentially life-threatening arrhythmias include the use of 3% mepivicaine or 4% prilocaine.
Angina pectoris is defined as severe pain in the chest caused by the relative deficiency of oxygen supply to the heart muscle. It occurs most often after increased activity, exercise, or a stressful event. Pain or numbness typically radiates to the left shoulder and down the left arm, and may also radiate to the neck and jaw. Discomfort of myocardial ischemia is described as squeezing, crushing, burning, or smothering, whereas others may describe it as a shortness of breath or simply a feeling of heaviness.
Clients who have the stable form of angina without a history of infarction generally have a much lower risk of complications than clients who have unstable angina or a history of a recent myocardial infarction. It is important to postpone elective treatment in those clients who have had a cardiac episode within the last 6 months. If the procedure is considered an emergency and cannot be postponed, consultation with the client’s cardiologist is of utmost importance. The risk of a second infarction drops as low as it will about 6 months after the initial myocardial infarction. It is recommended to consult with the cardiologist even after 6 months has passed.
Coronary artery bypass surgery is one of the most common surgical procedures performed in the United States today. Clients who have had coronary artery bypass surgery are treated in a manner similar to post-myocardial infarction clients. Six months should pass before any elective surgery or dental treatment is performed, and a consultation with the medical physician is recommended.
Percutaneous transluminal coronary angioplasty (PICA) is one treatment for coronary artery disease. After successful angioplasty, clients are maintained on aspirin therapy, which may interfere with clotting during dental surgery; therefore, a consultation with the physician is suggested prior to any treatment.
Congestive heart failure and orthopnea are common among older clients. Fatigue is a common complaint as well as a history of edema and weight gain from water and salt retention. Clients with congestive heart failure that is well compensated through dietary and drug therapy can safely undergo ambulatory surgery. Supplemental oxygen to assist with respiration and anxiety-reduction methods are helpful. Clients with congestive heart failure and orthopnea must be kept in an upright position during any procedure. Surgery for clients with uncompensated hypertrophic cardiomyopathy is best deferred until compensation is achieved or surgical procedures can be performed in a hospital setting. Appropriate analgesic agents for pain control or antibiotics for infection should be given after consultation with the client’s physician.
Clients with arrhythmias before dental surgery have significantly increased risks of cardiac morbidity and death. Clients with arrhythmias should be referred to a hospital-based oral surgeon or general dentistry program. In the hospital setting, appropriate consultation can be obtained to optimize the client prior to surgical treatment, which may be completed in one visit. Antiarrhythmic drugs are normally continued orally through the morning before surgery, after which medications will be delivered intravenously. Pacemakers pose no contraindications to dental surgery and no antibiotic prophylaxis is required, but electrical equipment such as electric cautery should not be used.
Infective Endocarditis
Infective endocarditis occurs when bacteria enter the bloodstream from an oral or other source and settle on heart valves that may already bear platelet fibrin thrombi. The frequency of bacteremia after different dental procedures or activities varies. After dental extractions or periodontal surgery it is quite high, approximately 18% to 85% and 32% to 88% respectively, but it also is significant after everyday activities such as toothbrushing, 0 to 26%, and chewing candy, 17% to 51%. The production of extracellular dextran by some strains of the streptococcus bacterium is responsible for the stickiness to dental enamel and also the culprit in trapping circulating organisms on damaged heart valves and platelet fibrin thrombi.
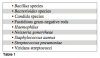
The mitral valve is the most common site of infection and once infection begins, rupturing of the valve tissue or chorda tendinae is possible. Some virulent bacteria (Staphylococcus aureus or some fungal infections) may become large enough to obstruct the orifice. Table 1 lists the bacteria most commonly associated with infective endocarditis.
Infective endocarditis can occur on either side of the heart. Some cases of streptococcal endocarditis can manifest clinically within 2 weeks of the initiating event. The dental team’s goal is to prevent endocarditis from occurring in susceptible clients. Any dental procedure that causes injury to the soft tissue or bone resulting in bleeding can produce a transient bacteremia. For clients with a history of infective endocarditis, antibiotic prophylaxis should be given.
In 2007, the American Heart Association changed its recommendations for short-term dental antibiotic prophylaxis. The American Heart Association along with the American Dental Association established the current guidelines for dentistry based on growing scientific evidence that shows the risks of taking preventive antibiotics outweighing the benefits for most dental patients. Some of the risks included adverse reactions to the prescribed antibiotics ranging from mild to potentially severe and, in very rare cases, death. Inappropriate use of antibiotics has also lead to the development of drug-resistant bacteria, a growing concern in the medical community. The new guidelines are aimed at patients who would have the greatest danger of a bad outcome if they developed a heart infection. Under the new guidelines, individuals who have taken antibiotics prior to dental treatment routinely in the past but no longer need them include conditions such as:
- bicuspid valve disease.
- calcified aortic stenosis.
- congenital heart conditions (ventricular septal defect, atrial septal defect, and hypertrophic cardiomyopathy).
- mitral valve prolapse.
- rheumatic heart disease.
Preventive antibiotics prior to a dental procedure are still advised for patients with:
- artificial heart valves.
- a history of infective endocarditis.
- certain specific, serious congenital heart conditions, including:
- unrepaired or incompletely repaired cyanotic congenital heart disease, including those with palliative shunts and conduits.
- a completely repaired congenital heart defect with prosthetic material or device, whether placed by surgery or by catheter intervention, during the first 6 months after the procedure.
- any repaired congenital heart defect with residual defect at the site or adjacent to the site of a prosthetic patch or a prosthetic device.
- a cardiac transplant that develops a problem in a heart valve.
Table 2 lists the types of antibiotics used and their dosages.
For the emergency client with one rheumatic fever episode with uncertainty about residual damage to the heart, a preventative prophylaxis should be administered prior to performing the procedure with a referral to the client’s physician for a consultation.
Hypertensive Disease
It is estimated that approximately 1.8 million adults in the United States develop hypertension annually. Hypertension is clinically defined as an average systolic blood pressure on a single occasion of >140 mm Hg or a diastolic blood pressure of >90 mm Hg. Isolated systolic hypertension is more commonly seen in older adults, whereas systolic and diastolic hypertension is more common in men under age 55, women over age 55, African Americans of all ages, and persons from lower socioeconomic groups.
Hypertensive clients should be treated in an anxiety-free atmosphere in order to prevent elevation of blood pressure to dangerous levels. Care must be taken in the administration of epinephrine or other vasoconstrictors to these clients, especially if a large amount is to be administered over a short period of time. Clients with severe uncontrolled hypertension should be identified and seen for conservative treatment in an anxiety-free environment only and referred to a medical physician before any surgical treatment is considered. Stress from dental procedures may increase the client’s already elevated blood pressure to a dangerous level and a medical consult is recommended.
Pulmonary Conditions
Chronic obstructive pulmonary disease (COPD) is a disorder characterized by abnormal tests in expiratory flow that do not change markedly over periods of several months’ observation. Specific causes of airflow obstruction—such as localized disease of the upper airways, bronchiectasis and cystic fibrosis—are excluded. COPD is a chronic disease that has its origins in early adulthood and possibly even early childhood. The disease does not produce symptoms or impairment of activity until it is far advanced, usually in late middle age or in the elderly. Surgical treatment should be rendered in an upright position to avoid orthopnea and respiratory discomfort. There is no contraindication to the usual usage of local anesthetics, however bilateral mandibular blocks or bilateral palatal blocks are not recommended because of a possible unpleasant choking sensation or difficulty in swallowing. Outpatient general anesthesia is contraindicated in clients with COPD.
Asthma is a disorder characterized symptomatically by cough, chest tightness, shortness of breath, and wheezing associated with limitation in airflow. The symptoms may be acute and episodic, or may wax and wane over long periods of time. Approximately one in 20 residents of the United States has asthma, and it is even more common in other developing countries. Approximately half of the asthmatics in the United States have onset of the disease during childhood, and about half will outgrow the disease by young adulthood. The goal of the dental team is to prevent an acute asthmatic attack. Aspirin ingestion is associated with a small percentage of attacks and it is advisable not to administer aspirin-containing medications or other NSAIDs to clients with asthma.
Acetaminophen can safely be used for mild to moderate pain. Barbiturates and narcotics should not be administered because of the potential of precipitating an attack. Nitrous oxide/oxygen sedation can be used because nitrous oxide is not a respiratory depressant or irritant. In cases where general anesthesia is to be used, treatment should be performed in a hospital setting.
Renal Diseases
Renal insufficiency can present either as a primary renal event or complicating another illness, and is a common clinical problem. There are currently more than 160,000 clients on dialysis in the United States and many more living with successful kidney transplants. Kidney diseases are often classified according to whether they produce acute or chronic renal failure. Clients with renal insufficiency requiring periodic dialysis need special consideration during oral surgical care. Clients with shunts should be given prophylactic antibiotics during surgery to prevent infection of the shunt. Elective oral surgery is best undertaken the day after a dialysis treatment has been performed. This allows the heparin used during dialysis to disappear and the client to be in the best physiological state with respect to intravascular volume and metabolic by-products. Drugs dependent on renal metabolism should be avoided or used in modified doses.
Disease of the Liver
Hepatitis is an inflammatory condition that may be localized in the liver or may be part of a generalized systemic disease. Acute hepatitis is usually a self-limited disease and the main causes include viruses, drugs, and alcohol. Chronic hepatitis refers to unresolved hepatitis that has persisted for longer than 6 months. Cirrhosis is often the main consequence of chronic hepatitis. Viral hepatitis is a systemic infection whose primary manifestations are hepatic. The six types of viral hepatitis that are well-defined, separate diseases are designated types A, B, C, D, E, and F.
The production of vitamin K-dependent coagulation factors (II, VII, IX, X) may be depressed in severe liver disease and obtaining a prothrombin time (PT) or partial prothrombin time (PPT) may be useful prior to surgery.
Diabetes Mellitus
Diabetes mellitus is a condition characterized by abnormal glucose utilization and associated with elevation of blood glucose concentration. The most common forms of diabetes mellitus are known to be associated with abnormalities of insulin secretion and concentration, with cellular resistance to insulin action, and with vascular abnormalities such as basement membrane thickening. Clients who have no evidence of complications and have their disease under good medical control will require little or no special attention when receiving surgical treatment, unless they should develop an acute dental or oral infection. Clients taking insulin and not under good medical management should be referred for a consultation before surgical treatment.
When a dentoalveolar procedure is scheduled for the morning, the client should be instructed to take the prescribed morning dose of regular insulin and half of the NPH (neutral protamine Hagedorn insulin) dose prior to the appointment. Vital signs should be monitored and the client observed for signs of mood change, tachycardia, hypotension, drowsiness, or hunger. Administration of oral glucose will counter the hypoglycemia. If the client will be unable to eat a normal meal following treatment, the morning dose of NPH should not be taken until regular meals can be eaten.
Infection in the diabetic client is more difficult to control than in clients without diabetes. This is a result of the altered leukocyte function, as well as by other factors that affect the body’s ability to control an infection. Difficulty in containing infection is more significant in clients with poorly controlled diabetes. In emergency situations involving the diabetic client with serious infections, hospitalization should be considered where appropriate doses of intravenous antibiotics could be administered and aggressive surgical management of the infection performed. Antibiotics may need to be given to diabetic clients when dental surgery is performed.
Thyroid Disease
One of the most common endocrine conditions is the disturbance of thyroid growth and function. Excessive production of thyroxine (T4) and triiodothyronine (T3) results in hyperthyroidism or thyrotoxicosis, while decreased hormone production results in hypothyroidism. Clients with hyperthyroidism should be referred to their physician before dental surgery. The hypothyroid client with mild symptoms can receive standard treatment.
Adrenal Insufficiency
Adrenal insufficiency is now most commonly caused by autoimmune disease and is associated with the presence of antibodies to adrenal tissue. Other cases are secondary to pituitary disease. A consultation with the physician of the client with adrenal insufficiency is recommended before dental surgical treatment. Minor procedures require anxiety-reducing measures whereas complex procedures may require supplemental steroidal treatment. A change in the client’s daily steroidal medication often occurs pre- and postoperatively.
Other Conditions
Alcoholism is a disease defined as a recurring trouble associated with drinking alcohol. The dental concerns when treating the alcoholic client are that of bleeding tendencies and unpredictable metabolism of certain drugs. Oral findings include gingival bleeding, glossitis, and loss of tongue papillae along with angular or labial cheilosis, which is complicated by concomitant candidal infections. Vitamin C deficiency and hemostasis disorder may lead to spontaneous bleeding, mucosal ecchymosis, and petechiae.
Inherited bleeding disorders are often reported to the dental team before treatment. For clients unsure if a bleeding disorder exists, questions about duration of bleeding following minor trauma or surgical procedures should be asked. A test of the intrinsic and extrinsic pathways, PT, and PPT is usually sufficient initially. In clients with a relative platelet inadequacy, a hematologist should be consulted. Clients with hemophilia A, B, C, or Von Willebrand disease should be given Amicar prior to any oral surgical procedure. Elective surgery should be planned with the hematologist to determine the best time for surgical procedures and whether transfusion of platelets will be needed. Table 3 lists normal hematologic values for tests normally given to clients with bleeding disorders prior to surgery.
HIV is a member of the lentivirus subfamily of human retroviruses. These retroviruses code for an enzyme known as reverse transcriptase. This enzyme allows transcription of viral RNA into proviral DNA and subsequent integration into the host’s cellular genome, leading to a persistent and latent infection.
Clients who are HIV-positive but asymptomatic can receive all indicated dental treatments. The physician should be consulted regarding the degree of immunosupression and thrombocytopenia. If the consultation is delayed, the client can be treated conservatively with pain medication and antibiotics. If the medical consultation reveals significant immunosupression and thrombocytopenia, bleeding time or platelet count should be performed before any treatment, as the client may require platelet replacement.
Joint replacement risks can be similar to that of infective endocarditis without prophylactic antibiotics, and these guidelines have not changed. The bacteria commonly found in the oral cavity may travel through the bloodstream and settle at the artificial joint, increasing the risk of contracting an infection. For the first 2 years after a joint replacement, all patients may need antibiotics for all high-risk dental procedures. High-risk dental procedures include extractions, periodontal procedures, regular cleanings if bleeding is anticipated, and some endodontic procedures. After 2 years, only high-risk patients may need to receive antibiotics for high-risk procedures.
Pregnancy risks include injury to the fetus, so no modifications that can cause genetic damage should be undertaken. All elective procedures should be postponed until after delivery. If surgery cannot be postponed, the client’s physician should be consulted before any treatment. Any drug to be prescribed must be discussed with the physician. The client should be seated in a nearly upright position or turned slightly to one side to prevent compression of the inferior vena cava. Nitrous oxide should not be used in the first trimester, but can be used in the second and third trimesters with at least 50% oxygen. Lidocaine, bupivicaine, acetaminophen, codeine, penicillin, and erythromycin can be used in moderate amounts. In the postpartum phase, if the client is breast-feeding, avoidance of drugs that enter the milk is necessary and the client’s physician should be consulted for guidance. Corticosteroids, aminoglycosides, and tetracyclines should be avoided entirely.
Seizure disorders are often identified by the medications listed on the client health assessment. Questions about frequency of medications, compliance, and any recent measure of drug levels should be asked. If the client is unable to answer any of these questions, treatment should be postponed and the physician consulted. If the client’s disorder is well-controlled, no special modifications are necessary. If the disorder is not well-controlled or if control cannot be attained, the client should receive intravenous sedation in an ambulatory setting, either at an oral surgery office or in the hospital.
REVIEW OF REGIONAL SURGICAL ANATOMY
The most important aspect of oral and maxillofacial surgery is a detailed knowledge of the regional anatomy. An inadvertent injury to a nerve will result in great morbidity to the client, and in a majority of the cases, legal challenges to the surgeon. The second and third divisions of the trigeminal nerve are the nerves most affected in oral surgery.
Nerves
The maxillary nerve is made up of three divisions: the pterygopalatine nerve, the infraorbital nerve, and the zygomatic nerve. The pterygopalatine nerve has several divisions, but the two terminal branches are most significant to dentistry. The larger of the two terminal branches is called the anterior palatine nerve and it enters the oral cavity through the greater palatine foramen. At this location it splits into several smaller branches fanning out as the greater palatine nerve and supplying the mucosa of the hard palate to the canines. The nerve travels next to the palatine artery contained by the connective tissue between the periosteum and the palatal mucosa. Injuries to the nerve endings within the palatal mucosa tend to repair themselves and clients will not usually be aware of any deficits in the nerve. This palatal tissue heals rapidly and sensory perception is not lost. The smaller branch of the pterygopalatine nerve is the posterior palatine nerve, which travels through the lesser palatine foramen, supplying the tonsil with sensory endings.
The infraorbital nerve divides out into three branches before it surfaces at the infraorbital foramen. These branches are called the anterior, middle, and posterior superior alveolar nerves, and supply sensory endings to the maxillary teeth, their periodontal membranes, and gingiva on the lateral aspect of the maxilla. In the base of the alveolar process, the superior alveolar nerves form a loose plexus called the superior dental plexus. The nerves in this plexus are the nerves anesthetized via infiltration of local anesthesia. Surgery in this region will not lead to any sensory deficits.
The terminal branches of the infraorbital nerve spread fan-like from the infraorbital foramen toward the lower eyelid, nose, and upper lip. Three or four superior labial branches enter the lip between the muscles and mucous membrane, supplying the mucosa of the upper lip and skin through perforation in the orbicularis muscle. Surgical disruptions of the terminal branches ending in the lip will repair themselves. During apicoectomies on the upper canine or premolar teeth, or sinus lift procedures on the atrophic maxilla, care must be taken not to injure the nerve as it exits from the infraorbital foramen. Injury in this region will lead to a traumatic neuroma and the neurological deficit will be permanent.
The mandibular nerve is a mixed nerve made up of both motor and sensory fibers. Four sensor branches are organized into internal, middle, and external branches. The internal branch has two nerves called the buccal and lingual nerves, supplying large areas of the oral mucosa. The middle branch is the inferior alveolar nerve supplying the mandibular teeth, skin, and mucosal membrane of the lower lip and skin of the chin. The external branch is the auriculotemporal nerve, which is never anesthetized in dentistry.
The buccal nerve enters the oral cavity at the anterior border of the tendon of the temporalis muscle and travels forward and downward within the fascia of the outer portion of the buccinator muscle. Branches of this nerve go through the buccinator muscle and supply the majority of the mucosa of the cheek. The buccal nerve is not encountered during surgical procedures; however, it sometimes is the cause of pain perception during retraction when a buccal flap is laid in the third molar area. Local infiltration into this area will alleviate the sensation.
The lingual nerve carries sensory and taste fibers starting out in close approximation with the inferior alveolar nerve from which it separates, approximately 5 mm to 10 mm below the base of the cranium. This nerve lies anteriorly and slightly medial to the inferior alveolar nerve, following the lateral surface of the medial pterygoid muscle to the level of the upper end of the mylohyoid line at which point it curves sharply anteriorly to continue horizontally on the upper surface of the mylohyoid muscle into the oral cavity. In the most posterior part of the oral cavity the lingual nerve is superficial and may be seen visually through the lingual mucosa above the mylohyoid line at the level of the third and second molars. Near the first molar, the nerve turns medially and goes underneath the submandibular duct, at which point it divides into several branches that enter the tongue.
The most exposed point for injuring the lingual nerve is medial to the retromolar trigome, and usually occurs during the removal of impacted third molars, especially in those clients who have had several episodes of pericoronitis. Multiple infections in this region can cause tissue contraction that pulls the nerve laterally onto the alveolar crest. Research has found that an anomalously high position of the lingual nerve relative to the internal oblique ridge occurs in approximately 10% of dental clients. Full recovery of neural sensation following an injury in this location is unlikely. Injuries of the nerve may also occur during the removal of sialoliths or any other surgery in the floor of the mouth. Following injury to the lingual nerve, surgical exploration and surgical repair is indicated when there is no evidence of recovery 30 days after the initial trauma. An 80% success rate of non-painful sensory return can be expected from microsurgical repairs of the lingual nerve if surgery is performed within the first 90 days following injury.
The inferior alveolar nerve enters the mandible at the lingula and travels through the length of the mandibular canal at which point it divides in the premolar region into the incisive and mental nerves. The mental nerve exits the mandible through the mental foramen where it divides into three to five branches. The incisive branch of the nerve continues within the mandible as part of the inferior dental plexus. These nerves supply the teeth and periodontal ligaments of the mandibular teeth. The relative position of the lingula varies with the age of the client, beginning more posterior and superior on the ramus as the mandible grows. The inferior alveolar nerve will be bordering the apex of the teeth in the third molar region and closest to the inferior border of the mandible beneath the roots of the first molars.
In the premolar region, the nerve is midway between the roots and the inferior border of the mandible. Surgical procedures planned in this area should have a panoramic film done prior to treatment to view the exact location of the nerve. The inferior alveolar canal is located approximately 4 mm to 7 mm from the lateral cortical cortex of the mandible. Injury to the nerve in this region occurs most often during third molar surgery. The location of the nerve in the bony canal aids in the regeneration of the nerve and return of sensation if fractured fragments of the canal do not block the canal. Usually 3 months is given for regeneration before microsurgical repair is considered. There is a significant association between the ages of the client and the permanency of persistent neurosensory deficits. In clients over the age of 40 with inferior alveolar nerve injury, 47% will have functionally problematic deficits such as lip biting and drooling more than 50% of the time. Presurgical counseling regarding persistent, functional, neurosensory problems should be stressed in clients over 40 years of age. Age is considered a contraindication in the removal of asymptomatic impacted third molars.
Table 4 outlines the major nerves involved in oral surgery.
Maxilla
The floor of the nasal cavity and the floor of the maxillary sinus influence minor surgical procedures on the maxillary alveolar region. Typically, the maxillary incisors are positioned below the floor of the nasal cavity, the maxillary premolars and molars are below the floor of the maxillary sinus, and the maxillary canines occupy a neutral position between the two cavities. The relationship of the apices of the incisors to the nasal floor will depend on the length of the incisor roots and the height of the alveolar process. The proximity of the teeth to the maxillary sinus is dependent on the alveolar recess of the maxillary sinus.
Cystic lesions, abscess arising from the incisors, or other pathology occurring in the anterior maxilla may bulge into the nasal cavity and could erode the nasal floor to involve the nasal mucosa. During surgery, the nasal mucosa will appear grayish in color when compared to the oral mucosa.
The maxillary sinuses are located within the maxillary bones immediately below the orbits on each side of the lateral walls of the nasal cavity. They are the largest of the paranasal sinuses and vary greatly in shape and size. They are pyramidal in shape with the base of the pyramid being the lateral wall of the nasal cavity. The apex of the pyramid points toward the zygoma, the pterygopalatine fossa forming the posterior wall, and the anterior wall of the maxilla forming the anterior wall of the pyramid. Maxillary sinuses are asymmetrical and often vary in size and shape within the same individual.
The palate is concave with the curvature being greater in the transverse direction. The hard palate is skeletal and makes up the bony palatine shelf of the maxilla and its overlying mucosa. Immediately beneath the mucosa are fat globules and mucous and mixed gland of varying sizes. Beneath the gland of the hard palate on either side of the palatal vault lie the greater palatine arteries, nerve, and vein. Surgical interventions on the hard palate are usually well tolerated and will present little anatomic challenge. Palatine tori are common occurrences and overaggressive surgical removal of a palatine torus may result in an oronasal fistula. The soft palate is muscular and dental surgery is rarely done in this area.
The edentulous maxilla sees many changes over time. The palatal vault will become shallower, and the anterior portion of the alveolar crest will show resorption in an upward and posterior direction. This occurs because the loss in the anterior portion of the maxilla is mostly on the labial and inferior aspect of the alveolar ridge. Following the loss of teeth, the maxillary sinus may expand into the alveolus from which teeth were lost. Recess of the sinus may reach far downward, becoming very thin. It is common to see as little as 3 mm of alveolar bone below the sinus floor. In severe cases, the nasopalatine neurovascular bundle may end up on the alveolar crest itself and the anterior nasal spine may be almost level with the alveolar crest. Crestal incisions in this region are placed toward the buccal so as to avoid the nasopalatine structures.
Upper lip support is progressively lost as the anterior maxilla decreases in size, tending to give the face a concave look or Class III facial appearance and Class III ridge relationship.
Mandible
The most significant structure that should be considered in mandibular surgery is the inferior alveolar nerve.
The medial shift of the alveolar process in the relationship to the bulk of the mandible causes the erupted third molar to lie in close proximity to the lingual cortical plate with a slight lingual inclination of its axis. The external oblique ridge contributes significant mass to the outer surface of the mandible in this area, and there is a thick layer of cancellous bone between the tooth socket and the outer cortical plate. There is also a lateral flare of the vertical ramus in relationship to the horizontal direction of the alveolus.
Impacted third molars bring the tooth very close to the mandibular canal. When the tooth becomes impacted against the distal aspect of the second molar or by the bone of the ascending ramus, the roots will grow deeper into the bone and will get close to the inferior alveolar canal or may even grow beyond the level of the canal.
The root and canal will rarely meet because in most cases the impacted third molar is lingually inclined and the roots pass the canal on the buccal side. In cases where the crown of the molar is buccally inclined or in distoangular impactions, the roots may be right above the canal. In an attempt to remove these types of teeth by applying an instrument that exerts pressure distally, the force may lead to a fracture of the roof of the canal that may leave residual bony fragments to impinge on the neurovascular bundle. This type of nerve injury is persistent if the pressure is not relieved.
The first premolar is in close approximation to the mental nerve. Any surgical procedures done in this area may damage the nerve. Incision and drainage of an abscess, apicoectomies, buccal flaps, and other surgical procedures may damage the mental nerve. The mental canal arises from the mandibular canal in the area of the first premolar. This short canal runs outward, upward, and backward to open at the mental foramen located between the two premolars or below the root of the second premolar. The mental nerve is situated in the periosteum that is tightly bound to the opening of the foramen and forms a thick collar around the nerve.
One of the most significant changes in an edentulous mandible is that the mental foramen becomes closer to the crest as the alveolar process decreases in height. As a result, the mandibular nerve is more susceptible to injury during any attempted preprosthetic surgery in the area. In severe cases of resorption, the mandibular nerve, the mental nerve, and the genial tubercle may all be located superior to the crest of the mandible. In bone loss progression, vertical dimension is lost resulting in an increasingly Class III facial form and maxillomandibular jaw relationship. The mentalis muscle insertion on the mandible may be lost, resulting in a lifting of the muscle and mucosa above the level of the alveolar ridge. This muscle pull also has a tendency to roll the lower lip toward the alveolar ridge, consequently decreasing the amount of alveolar ridge exposed in the oral cavity.
ANESTHESIA AND SEDATION
Defining and understanding the levels of dental anesthesia and sedation are important because the different stages represent different degrees of possible risk. Prior to administration of anesthesia/sedation to a dental client, one must understand that the sedative effects of drugs represent a continuum of dose-related responses. These responses can vary from light sedation to intense central nervous system depression to death.
Normal Activity
Light Conscious Sedation
Deep Sedation
General Anesthesia
Coma
Death
An individual client’s response to sedation relies not only on the dose of the drug but also on the sensitivity of that client to the particular drug. An identically given dose of the same medication to two different individuals can have two different effects.
There are three definitions of pain and anxiety control techniques:
- Conscious sedation is defined as a minimal level of consciousness that retains the client’s ability to independently, continuously maintain an airway, and respond appropriately to physical stimulation and verbal commands. A pharmacological or nonpharmacologic agent or a combination thereof produces this consciousness.
- Deep sedation is defined as a controlled state of depressed consciousness, accompanied by a partial loss of protective reflexes including the inability to continually maintain an airway independently and/or respond purposefully to verbal commands. A pharmacological or nonpharmacologic agent or a combination thereof produces this consciousness.
- General anesthesia is defined as a controlled state of unconsciousness accompanied by a partial or complete loss of protective reflexes, including the inability to independently maintain an airway and respond purposefully to physical stimulation or verbal commands. A pharmacological or nonpharmacologic agent or a combination thereof produces this consciousness.
Preoperative Client Evaluation
When a client requires in-office parenteral sedation, the surgeon and anesthetist must thoroughly and accurately evaluate the client. This evaluation is divided into three parts, the history, brief physical examination, and laboratory screening tests as indicated.
The medical history is the single most important aspect of the client evaluation, as discussed earlier in this course under Client Health Assessment and Vital Signs.
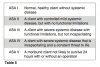
The next phase is the brief physical evaluation with focus on the respiratory, cardiac, and neurological systems. This evaluation often includes blood pressure, pulse rate and rhythm, respiratory rate, and weight. Auscultation of the lungs is necessary in clients with any significant pulmonary disorders in order to evaluate current respiratory condition. Significant pulmonary disorders include asthma, recent respiratory infections, COPD, and heavy smoking. A cardiac auscultation should be performed if there is a question of a heart murmur or heart valve abnormality. At this point, the client is assigned a physical status category according to the American Society of Anesthesiologists (ASA) physical status classification status (Table 5). Clients who fall into the ASA I categories and II pose no unusual risks in undergoing properly administered office sedation. Clients in categories III and IV may require additional evaluation, including specific laboratory tests and/or a consultation with the medical physician. Some clients may not be suitable for in-office sedation and may be referred to the hospital for treatment.
The third component of the client evaluation is the use of laboratory screening tests. It is the most controversial and least utilized component of the client evaluation. Clients with systemic disease should have the appropriate diagnostic tests based on the severity and type of medical condition.
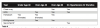
The recommended types of laboratory tests are shown in Table 6.
Preparatory Steps Before Surgery
Preparing the client for dental surgery is often delegated to the dental assistant. For every client, the vital signs need to be assessed. In clients who are only having local anesthesia, only the blood pressure needs to be taken. The basic preparatory steps before surgery include:
- Verification that the client consent form is accurate and has been signed.
- Confirmation that a driver is present for sedated clients.
- Contact lens wearers are asked to remove their lenses if sedation or general anesthesia is being used.
- Verification that all prescribed medications has been taken.
- Confirmation of client height and weight to determine anesthetic dosages.
- Review and confirm information on the health assessment form.
- Determine whether a female patient is pregnant or taking oral contraceptives.
- Determine when last meal was eaten for clients who are to be sedated or receive general anesthetic.
- Check and record vital signs before and after the surgical procedure.
- Connect all monitors.
- Provide an antimicrobial rinse before seating the patient.
- Assist with the administration of all forms of anesthetic.
Client Monitoring
The monitoring of clients undergoing sedation can be done by a dental auxiliary or by a machine. It is important that monitoring is done throughout the procedure to recognize abnormal changes in respiration, cardiac rhythm, and circulation before serious complication arise.
The respiratory system is monitored differently in a nonintubated client, the type most likely to be found in dental clinics, than in clients who are intubated. Observation of the chest rising and falling with each breath or the movement of the reservoir bag during inhalation and exhalation can easily be done in the nonintubated client. In the intubated client, a capnograph is the most accurate way of measuring end-tidal CO2. A pulse-oximeter measures the ratio of saturated and desaturated arterial blood and displays the relative saturation value, SaO2. SaO2 values of 90% and higher are acceptable. Most new pulse-oximeters have an alarm that can be set to sound when the SaO2 value drops to 90% to warn against impending hypoxia.
Monitoring of the cardiovascular system involves the ability to assess blood pressure, cardiac function, and circulation. Heart rate, dysrhythmias, and ischemic changes are monitored with an electrocardiogram (ECG). Pulse-oximeters can monitor the heart as well as oxygen saturation. Tachycardia and bradycardia are conditions of concern and often are points set internally in the alarm system. Blood pressure can be monitored by a manual or automated sphygmomanometer. These automated machines can be set to take the blood pressure and pulse at any desired minute interval.
Sedation should also include a record of anesthesia as well as procedure notes for the services rendered. Most anesthesia records are abridged versions of the ones anesthesiologists in hospitals use. These versions allow for recording the time drugs are given, pulse, blood pressure, SaO2, and ECG in graphic format. Basic information—such as client name, age, weight, ASA classification, medications, monitors, procedure, surgeon, and vital signs every 5 to 15 minutes—is also included in the records.
Administration Techniques
There are numerous routes of administration available for sedation techniques in oral and maxillofacial surgery, including inhalation (IH), oral (PO), submucosal (SM), intramuscular (IM), intravenous (IV), and rectal (PR). Of the previous six modes of administration, the rectal (PR) is rarely used in oral surgery procedures.
For conscious sedation, inhalation techniques are limited to nitrous oxide–oxygen. The ease of use, rapid onset, and rapid recovery are advantageous. The two major disadvantages include its relative impotence and interference from the nasal hood during the procedure.
Oral administration is the easiest and most convenient sedation technique, but it is also the most unpredictable. The unpredictability is the result of the effects of gastric enzymes, stomach contents, rates of emptying, and gastric absorption on the drug administered. Many of the drugs are foul-tasting and can produce vomiting following ingestion, affecting the actual dose absorbed.
The number of drugs used that can be administered subcutaneously for conscious sedation are few and most of those drugs are too irritating and would cause tissue sloughing. Two useful drugs that can be safely administered subcutaneously in the oral cavity are atropine and succinylcholine.
Intramuscular administration has the second most rapid rate of absorption of a parenterally administered drug, with only intravenously administered drugs acting more quickly. There are three anatomic areas suitable for IM administration: the most common site is the buttock, specifically the gluteus medias muscle; the vastus lateralis muscle of the lateral aspect of the anterior thigh; and the deltoid muscle of the upper arm.
Intravenous administration allows introduction of the drugs directly into the bloodstream, resulting in the most rapid effect. IV administration bypasses the problems of variable absorption and achieves the most predictable and consistent blood levels. Sedative agents can be given in small doses, called titration, to reach a desired effect. Three types of cannulas are available for IV administration: the traditional hollow “straight” needle, a winged or “butterfly” needle, and a plastic catheter. The basic technique of venipuncture is the same for all three types of cannulas.
Preparing Medication from a Multi-Dose Vial
In some offices, the oral and maxillofacial surgery assistant may have to prepare the medication syringes. Some oral and maxillofacial surgeons use manufactured prefilled syringes, but most use multidose vials and draw up the needed amounts of chemical agents into each syringe. Each syringe must be labeled so that the chemical agents are not administered incorrectly. These syringes should be kept in a locked cabinet for protection and when specified by law. When a chemical agent syringe is prepared, the assistant should verify the expiration date, read the label before filling the syringe, and read the label after filling the syringe to ensure that the proper chemical agent has been prepared. When preparing syringes from a multidose vial, the basic steps include:
- Wipe the rubber diaphragm on the top of the vial with an alcohol sponge and dry it with a sterile sponge.
- To withdraw liquid from the vial, pull back on the plunger of the syringe until it reaches the specific graduation mark that indicates the proper amount of agent to be used.
- Hold the vial with the diaphragm facing the floor, remove the needle cap, and pierce the rubber diaphragm.
- Push down on the plunger, ejecting the air into the vial.
- Pull back on the plunger to withdraw the correct amount of agent to fill the syringe.
- If bubbles enter the syringe during filling, gently tap on the side of the syringe with the needle end of the syringe pointing upward.
- Expel the bubbles by gently pressing the plunger forward.
- After the syringe is filled with the correct amount of the agent, withdraw the needle from the vial and recap using a capping device or one-handed scoop method.
- If additional agent is needed, repeat the process with a sterile syringe.
Preparing the IV Bag
An assistant may be asked to prepare the IV bag and chemical agents. IV bags come in several sizes with the most common being 250 mL, 500 mL, and 1000 mL. Basic instructions for preparing the IV bag include:
- Open and remove the packaging on the IV bag.
- Hold the port end of the bag upside down so that the fluid cannot leak out, and pull the seal from the neck of the bag.
- Remove the protective cover from the pointed end of the drip chamber of the IV tubing set and with a twisting motion insert it into the port of the IV bag.
- Turn the bag so that the port and the IV tubing are at the bottom.
- Place the bag on the stand and gently squeeze the drip chamber of the IV tubing, filling it approximately half full.
- Remove the protective covering at the opposite end of the IV tubing and allow the fluid to flow through the tube.
- When the fluid reaches the end, tighten the adjustable clamp to stop the flow of fluid.
- Replace the protective cover over the end of the tubing until it is attached to the IV cannula in the client’s arm.
Local Anesthesia
Every oral and maxillofacial surgery procedure must include local anesthesia. Local anesthesia is a reversible blockade of nerve conduction in a specific area that produces loss of sensation and motor activity. The anesthetic agents stabilize neural membranes by inhibiting the ionic influxes required for propagation of neural impulses. Local anesthesia also controls bleeding during surgery and aids pain control immediately after the procedure. Current chemical agents used to produce local anesthesia are classified as either an ester or an amide. They are further classified according to their duration of action.
Short-acting Less than 2 hours
Moderate-acting 2 to 4 hours
Long-acting 4 to 18 hours
The duration of the planned surgical procedure along with the anticipated need for postoperative pain control guide the surgeon in which type of anesthetic to use.
Inhalation Analgesia/Sedation
Nitrous oxide is used readily in all aspects of dentistry. The gas is a colorless, nonirritating gas with a mild, slightly sweet odor. Nitrous oxide has a blood/gas partition coefficient of 0.47 and therefore is poorly soluble in the blood. It is excreted unchanged by the lungs and rapidly equilibrates between alveolar and arterial concentration gradients. Because of this, both induction and emergence times are very short. The primary disadvantage of using nitrous oxide is its lack of potency. The highest safe concentration of nitrous oxide is 80%, the remaining 20% being oxygen, the same concentration of oxygen found in room air. At this high concentration of nitrous oxide, the deepest plane of analgesia achieved is analgesia, or Stage I. At nitrous doses of 30% to 40%, excellent analgesia is reached. Sixty percent is generally considered the maximum concentration for good analgesia while still allowing the client to maintain verbal contact with the clinician. At rates of 30%, the analgesic effect of nitrous oxide is comparable to 10 mg of morphine sulfate. At the conclusion of inhalation analgesia, 100% oxygen must be administered for a minimum of 3 minutes in order to prevent diffusion hypoxia. This occurs as a result of large volumes of nitrous oxide diffusing out quickly into the alveoli of the lung diluting the available oxygen and reducing the alveolar oxygen concentration. Another cause for hypoxia is the dilution of alveolar carbon dioxide, resulting in decreased respiratory drive and ventilation.
A scavenging system is essential for the safety of the clinic personnel. This system removes waste gases and prevents their disbursement into the room air. In some states, the expanded function of nitrous oxide monitoring can be delegated to the dental assistant. In other states, actual administration can be delegated with additional education.
Chemical Agents Used In Oral and Maxillofacial Surgery
There are many chemical agents that are used in oral and maxillofacial surgery for sedation. The prototypical narcotic is morphine sulfate, although it is rarely used now for sedation.
Barbiturates have been used since 1960, particularly methohexital (Brevital) for the induction of general anesthesia as well as an anesthetic maintenance agent for brief surgical procedures. Methohexital is a short-acting barbiturate and the most commonly used agent by oral and maxillofacial surgeons for office-based outpatient sedation. Compared with its predecessors, thiamylal (Surital) and thiopental (Pentothal), methohexital is twice as potent with one half the duration of action. The central nervous system effects of barbiturates are not fully understood although they seem to depress the ascending neuronal activity through the reticular activating system in the brain. The degree of depression is dose-related, and there is no analgesic effect of barbiturates; on the contrary, it is thought that these agents are anti-analgesic and may enhance painful stimuli. There is no specific reversal agent for barbiturates.
Methohexital comes as a freeze-dried sterile powder that is reconstituted with sterile water or normal saline solution. Diffusion into the brain is quick—within 30 seconds of intravenous administration. The short duration of the drug is a result of its quick redistribution into the skeletal muscles, adipose tissue, and other vessel-poor groups. Because the drug does not accumulate in the adipose tissue, cumulative effects are less and recovery is faster than with other barbiturates. Methohexital is eliminated through the liver via demethylation and oxidation and excreted by the kidneys. Barbiturates including methohexinal produce a dose-related depression of the medullary and pontine areas of respiratory control. They also decrease the brain’s sensitivity to blood pH and CO2 levels and depress the chemoreceptors in the carotid and aortic bodies to O2 concentration.
Benzodiazepines were introduced into outpatient sedation in the 1960s and currently dominate the field as both single agents and as part of multiple-agent techniques. Introduced in the 1980s, the two most popular benzodiazepines are diazepam (Valium) and midazolam (Versed). Benzodiazepines act directly on the limbic system, thalamus and hypothalamus, and also interact with the gamma aminobutyric acid (GABA) receptors. Although these receptors are the sites of action of the drug and are responsible for the calming and antiemetic effect, euphoria, amnesia, and muscle relaxation, there are no essential analgesic properties. The cardiac effects of benzodiazepines are small and often this drug is used in cardiac clients as premedication and part of the induction sequence for general anesthesia. The respiratory effects of benzodiazepines are the most serious when administered as part of conscious sedation because tidal volume is decreased and the respiratory rate increases. Midazolam is contraindicated in clients with pre-existing diseases such as COPD, and has a greater effect in depression of tidal volumes. All benzodiazepines are contraindicated in clients with glaucoma.
Diazepam is mixed with propylene glycol and ethyl alcohol prior to intravenous use because of its water insolubility. Use of diazepam can be irritating to vascular vessels and is not used in the small veins of the wrist or backside of the hand. This drug is not mixed with any other drug and is administered slowly, at a rate of 1 mL per minute. Peak onset is 3 to 5 minutes. The drug accumulates in the body fat and then is slowly re-released into the circulatory system, and then ultimately metabolized. Duration of diazepam is prolonged with the drug’s half-life of 20 to 50 hours.
Midazolam is shorter acting than diazepam and is soluble in water and less irritating to the vascular tissue. It is approximately two to three times as potent as diazepam and onset of action is dependent upon the drug used for premedication. Even though the half-life of midazolam is only 2 to 4 hours, clinical recovery time is the same as with using diazepam.
Ketamine was introduced into the dental field as an anesthetic in 1965 in Europe and in 1970 to the United States. At that time, ketamine was classified as an anesthetic that produced “dissociative anesthesia.” Ketamine is a derivative of phencyclidine, also known as PCP or “angel dust,” and is an acidic water-soluble solution that can be administered intravenously or intramuscularly. During IV administration, onset of dissociative anesthesia is 30 to 60 seconds at doses of 2 mg/kg, with duration lasting only 5 to 10 minutes. Administration should be over 1 minute to decrease the incidence of respiratory depression and/or a hypertensive response. When administered intramuscularly, at doses ranging from 9 mg/kg to 13 mg/kg, onset of surgical anesthesia is about 3 minutes with duration of 12 to 25 minutes. Half-life of ketamine varies from 1 to 2 hours in children and 2 to 3 hours in adults.
The central nervous system effects of ketamine are profound and “dissociative anesthesia” is characterized by intense analgesia, amnesia, and catalepsy. The dissociation component refers to the disruption of the pathways in the brain, preventing the higher cortical centers from receiving painful stimuli as well as auditory and visual signals. Emergency side effects can be reduced with intramuscular administration and include hallucinations and delirium. One advantage to using ketamine is that as long as administration is slow it has minimal negative respiratory effects, even at full anesthetic doses. Premedication is usually with atropine. Ketamine is used with caution in clients with coronary artery disease, but can be used safely in clients with asthma.
Narcotics act directly on the central nervous system, specifically on the microreceptors that depress ventilation, euphoria, sedation, and spinal analgesia. Used alone, narcotics will not cause the loss of consciousness in a young and healthy client. Meperidine (Demerol) has been used with success for many years in outpatient surgery. Doses range from 25 mg to 100 mg with sedative and analgesic effects that are useful both during the procedure and postoperatively. The actions of meperidine are similar to morphine, but have a quicker onset and shorter duration of action. Onset is typically 3 to 5 minutes, however it is only 15% as potent as morphine. In comparison with morphine sulfate, meperidine has less effect in depressing the cough reflex and is metabolized by the liver. Because meperidine can cause significant respiratory depression and release of histamines, its use is contraindicated in clients with asthma, and those who take or have taken monoamine oxidase (MAO) inhibitors within 2 weeks of the procedure. Effects of meperidine can be reversed with naloxone.
Reversal Agents
Currently, reversal agents exist only for the opioid and benzodiazepine classes of drugs commonly used for office-based sedation in oral and maxillofacial surgery. The only pure opioid antagonist available for parenteral use is naloxone (Narcan). Naloxone reverses all effects of opioids including respiratory depression, analgesia, hypotension, and sedation. Naloxone competitively binds to all of the various narcotic receptor sites in the central nervous system and the prenarcotized state is quickly restored. It can be administered through IV, intramuscularly or subcutaneously. The onset of action is approximately 2 minutes after IV injection, slightly slower with the other two methods of administration. The duration of action varies from 31 to 81 minutes and is dose and route of administration dependent. A total dose of 10 mg is considered a maximum reversal dose, no additional benefits are expected in greater quantities.
A recently available benzodiazepine-specific reversal agent, flumazenil (Romazicon) replaces other nonspecific agents previously used, such as physotigmine and aminophylline. Flumazenil is an imidazobenzodiazepine that is a pure benzodiazepine in humans. It reverses the effects on the central nervous system by competitively binding with the benzodiazepine receptors in the GABA complex. It does not inhibit other drugs such as barbiturates, ethanol, narcotics, and general anesthesia. Flumazenil delivered intravenously will reverse amnesia, sedation, psychomotor impairment, and respiratory depression. The degree and duration of the antagonistic effects is dependent on dose and plasma concentration over time. The reversal effects are evident within 1 to 3 minutes and peak effect is reached at 6 to 10 minutes. The half-life of flumazenil is approximately 60 minutes and resedation is possible when large doses of agonists are used. Flumazenil is recommended for intravenous use only and is packaged in multidose vials.
Sedation Techniques
Clients presenting for conscious sedation should have refrained from eating solid foods for 8 hours. Clear, noncarbonated liquids can be imbibed up to 3 hours preoperatively. The client is placed in a chair and all necessary monitors for the type of anesthesia planned are attached. Vital signs prior to any administration are taken and recorded. Nitrous oxide/oxygen inhalation is started via a nasal hood, gradually being increased to the desired level. IV access is obtained and continuous infusion is started. The anxyolitic agent, usually a benzodiazepine, is administered first. After waiting a sufficient length of time to gauge the anxyolitic agent’s effect, the analgesic agent is added, either a narcotic or ketamine. Finally, as needed on an individual basis, an amnesic agent in the form of a barbiturate is added.
MEDICAL EMERGENCIES DURING OUTPATIENT SEDATION
Recognition and management of medical emergencies is imperative during outpatient sedation. Associated complications that arise can be secondary to either the sedation and/or the surgical procedure. Table 7 lists some of the most common medical emergencies during outpatient sedation and their treatment modalities. Table 8 outlines how the bleeding mechanism works; Table 9 explains how to assess a patient’s bleeding risk preoperatively.
Perioperative Hemorrhage
Successful management of perioperative hemorrhage during dental surgery depends on three things:
- Preoperative identification of patients with a possible bleeding diathesis
- Minimization of blood loss during the surgical procedure
- Identification and elimination or correction of the causes of postsurgical bleeding and reestablishment of adequate hemostasis
Preoperative identification of patients with a possible bleeding diathesis is done with the client health assessment form. Drug usage, whether prescription or over the counter, is the most common undocumented cause of bleeding in surgical clients. Special emphasis must be placed on nonsteroidal anti-inflammatory drugs (NSAIDs) because they are currently the most widely used drugs that may cause bleeding. Anticoagulants and antibiotics are another important group of drugs that must be considered.
Major risk factors for surgical bleeding include:
- Bleeding with prior surgical procedure
- Extraction of teeth or periodontal surgery
- Excessive bleeding following any minor surgical procedure
- Obstetric bleeding
- Heavy menstrual flow
- Liver disease
- Hepatitis B and C
- Cirrhosis
- Chronic alcohol abuse
- Renal disease
- Known hereditary diseases
- Hemophilia
- Von Willebrand’s disease
- Other inherited coagulpathies
- History of abnormal blood counts
- Leukemia
- Thrombocytopenia
- Medication
- NSAIDs
- Aspirin
- Anticoagulants
- Antibiotics
- Chemotherapeutic agents
Minor risk factors to assess surgical risk for bleeding include:
- History of unusual bleeding
- Frequent episodes of epistaxis
- Unusual mucosal bleeding
- Abuse of illicit drugs
Bleeding disorders may be either intrinsic or acquired. Intrinsic disorders are inherited and bleeding results from congenitally deficient or dysfunctional components of the hemostatic system. Intrinsic bleeding disorders include Hemophilia A and B and Von Willebrand’s disease. Acquired disorders result because of an underlying condition or disease. Acquired bleeding disorders include decreased production of platelets and increased destruction of platelets. In addition, clients taking heparin, warfarin, aspirin, NSAIDs; and clients with liver disease or systemic diseases can acquire bleeding disorders.
Management of Specific Problems Affecting Hemostasis
Aspirin and NSAIDs are widely used groups of drugs. They are taken for many reasons, whether for chronic pain or used as an anticoagulant. Both drugs inhibit thromboxane A2 synthesis, causing a decrease in the ADP release and ultimately a decrease in platelet aggregation. Aspirin can inhibit platelet function even after as low a dose as 300 mg, and its effects can last for days until sufficient new platelets have been formed to correct the defect. Bleeding time is prolonged in these clients.
For clients on a low-dose aspirin therapy, consult with the physician in order to stop the drug 7 to 10 days before the surgical procedure. If the risk is too high to terminate therapy and the surgical procedure is minor, bleeding may be managed by local methods such as Gelfoam and Gelfoam soaked with thrombin. In these cases, the Gelfoam is placed in the extraction site and gingival margins are tightly secured with sutures. The sutures maintain pressure on the wound for initial hemostasis. For surgical sites where the use of Gelfoam is impractical, a layer of topical collagen may be used.
The effect of NSAIDs on platelets is quantitatively less and of shorter duration than aspirin. NSAIDs should be stopped 2 to 3 days before surgery.
Warfarin (Coumadin) is an anticoagulant used by many as a preventative measure for embolic phenomena related to several conditions. Some of the more common conditions include atrial fibrillation, dilated cardiomyopathy, systolic congestive heart failure with poor ejection fraction, valvular heart disease, metallic cardiac valve replacement, and deep vein thrombosis/pulmonary embolism prevention. Warfarin inhibits the production of vitamin K-dependent factors II, VII, IX, and X. The use of vitamin K to correct an acute bleed in this client population is contraindicated. Vitamin K will require 12 to 36 hours before the coagulating action can be seen. Vitamin K administration will make renewed oral anticoagulation very difficult for several days. This exposes the client to the risk of embolism.
Antibiotics used long term can cause defects in the coagulation system because of their effect on vitamin K production and absorption. A PT (prothrombin time) should be done. If the PT is elevated, these clients will benefit from the administration of vitamin K1. An initial dose of 15 mg to 20 mg intravenously will return the PT to normal within 6 to 12 hours. Usually a smaller dose of 10 mg intravenously or subcutaneously is used in controlling hemorrhagic episodes. The initial dose is followed by one third the dose every 8 to 12 hours. When vitamin K is given intravenously, care must be taken to administer slowly (<5 mg/min) to avoid the precipitation of a hypotensive episode.
Platelets play a key role in surgical hemostasis. An adequate quantity and satisfactory functioning of platelets is required for successful hemostasis. The platelet count is usually obtained as a part of the CBC (complete blood count). Normal platelet numbers are 190,000/μl to 400,000/μl. Thrombocytopenia in the range of 50,000/μl to 100,000/μl will increase the bleeding time, but is satisfactory for minor surgical extractions and biopsies. Elective oral surgical procedures should not be performed on clients with platelets less than 50,000/μl.
Hemophilia A/B and von Willebrand Disease are congenital coagulation disorders that should be managed in conjunction with a hematologist in a hospital setting.
Hemorrhage control during and after surgical procedures will be covered in part two of this course.
Summary
The number of people taking medications today is likely increasing. Many of these people will eventually need some form of surgical dental procedure. With thorough preparation, the surgical assistant can aid the dentist or surgeon. This course reviewed how to assess client health and risks for oral surgery procedures, whether performed in the general dentistry practice or specialty clinic. Although this course touched briefly on many important areas, only further study and proper training can fully prepare the surgery dental assistant.
References
Peterson LJ, et al. Contemporary Oral and Maxillofacial Surgery. 3rd ed. St. Louis, MO: 1998; Mosby.
Littel JW, et al. Dental Management of the Medically Compromised Patient. 5th ed., St. Louis, MO: 1997; Mosby.
Andreoli TE et al. Cecil Essentials of Medicine. 5th ed. Philadelphia, PA: 2000; WB Saunders.
Sicher H, DuBrul EL. Oral Anatomy. 6th ed. St Louis, MO: 1975; Mosby.
Gregg JM. Surgical management of lingual nerve injuries. Oral Maxillofac Surg Clin North Am. 1992;4(2):417-424.
Butterworth JF. Molecular mechanisms of local anesthetics: A review. Anesthesiology. 1990;72:711-734.
Bennett CR. Local Anesthesia and Pain Control in Dental Practice. 7th ed. St. Louis, MO: 1983; Mosby.
Jorgenson NB, Hayden S. Premedication: Local and General Anesthesia in Dentistry. Philadelphia, PA: 1967; Lea & Febiger.
Adriani J. The clinical pharmacology of local anesthetics. Clinical Pharmacology Ther. 1960;1:645-673.
Ring ME. Dentistry: An Illustrated History. St. Louis, MO: 1986; Mosby.
Nique TA. Preanesthethic evaluation of the ambulatory oral surgery patient. Oral Maxillofac Surg Clin North Am. 1992;4:743-751.
Rackow H, Salamitre E, Frumin MH. Dilution of alveolar gases during nitrous oxide excretion in man. J Appl Physiol. 1961;16:723.
University Of Minnesota Nitrous Oxide Course. Dr. James Swift – lecture notes, January 2001.
Peterson P, Hayes TE, Arkin CF, et al. The preoperative bleeding time test lacks clinical benefit. Arch Surg. 1998;133:134.
Caranasos GJ. Drug reactions. Principles and Practice of Emergency Medicine. 2nd ed. Philadelphia, PA: 1986; WB Saunders.
Malamed SF. Medical Emergencies in the Dental Office. St. Louis, MO: 1993; Mosby.
Smith RG, et al. Dental Surgery Assistants Handbook. 2nd ed. Bristol: 1993; Mosby.
American Heart Association Endocarditis Prophylaxis Information (2008). http://www.americanheart.org/presenter.jhtml?identifier=11086
American Dental Association (2003). http://www.ada.org/prof/resources/pubs/jada/reports/report_prophy_statement.pdf
American Dental Association (2007). New Guidelines from the American Heart Association. http://www.ada.org/public/topics/antibiotics.asp
About the Author
Natalie Kaweckyj is the clinic coordinator and compliance analyst for Children’s Dental Services, a non-profit community clinic serving the underserved in the Twin Cities. She is a Registered Dental Assistant in restorative functions, Certified Dental Assistant, Certified Dental Practice Management Administrator, Certified Orthodontic Assistant, Certified Oral & Maxillofacial Surgery Assistant, a Master of the American Dental Assistants Association, and holds several expanded function certificates including the administration of nitrous oxide/oxygen analgesia and orthodontic band removal. She is a past president of the American Dental Assistants Association.