You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
GLOSSARY
Acetone—waste product of cellular metabolism
Acidosis—acid condition in the blood or body fluids
AED—automatic external defibrillator
Agitation—mental confusion caused by hypoxia
Allergen—substance capable of causing an allergic reaction
Anaphylaxis—severe allergic reaction affecting respiration and heart function
Aneroid gauge—gauge or dial on a blood pressure cuff
Angina—chest pain related to exertion, emotion, or exercise
Angioneurotic edema—allergic swelling of the pharyngeal structures
Antecubital space—elbow space
Antibody—body chemical produced on exposure to germs or allergens
Antigen—substance capable of stimulating antibody formation
Antisialagogue—drug used to decrease secretion of salivary glands
Aphasia—inability to speak
Apnea—not breathing
Arrhythmias—irregularities or abnormal heart rhythms
Ascites—fluid accumulation in the abdomen
Aspiration—act of inhaling fluid or vomit into the lungs
Atherosclerosis—build-up of fatty deposits in the arteries
Benzodiazepines—class of drugs used to reduce anxiety
Brachial artery—artery that can be palpated on the inside of the antecubital space
Bradycardia—slow heart rate, less than 60 beats per minute
Bronchioles—small airway tubes within the lungs
Bronchitis—inflammation of the bronchi caused by irritation
Bronchodilator—drug capable of relaxing (dilating) the bronchioles
Bronchospasm—constriction or narrowing of the bronchioles due to muscle constriction
Carpopedal spasm—painful claw-like appearance of the hands seen in hyperventilation
Cerebral cortex—outer layer of the brain controlling higher functions (motor function, consciousness, sensation)
Circumoral—around the mouth
Clonic—repetitive muscle contraction and relaxation phase of a seizure
COPD—chronic obstructive pulmonary disease, a combination of emphysema and bronchitis
Cyanotic—bluish discoloration of the skin caused by low oxygen levels in the blood
Dehydration—condition caused by the abnormal loss of fluid from the body
Diabetes—disorder of sugar metabolism due to a lack of insulin
Diaphoresis—sweating
Diastole—relaxation phase of the heart cycle
Diastolic—the lower, or second, of the two pressures making up the blood pressure; the force of blood against the blood vessel walls during ventricular relaxation
Dyspneia—shortness of breath
Emphysema—chronic, progressive disease of the lung involving the smaller airways and air sacs
Epigastric—the upper portion of the abdomen
Epilepsy—neurological disorder associated with seizures
Exhalation—movement of air out of the lungs
Fibrinolysis—process when a clot or coagulation is broken down
Gingival hyperplasia—an overgrowth of gingival tissue often requiring surgery to reduce
Glaucoma—increased pressure in the anterior chamber of the eye which may lead to blindness
Glucose—form of sugar preferred by the body as an energy source for metabolism
HEPA respirator—High Efficiency Particulate Arresting; air respirator used for personal protection when working with patients with known or suspected tuberculosis
Hepatomegaly—swelling or enlargement of the liver seen in right heart failure
Histamine—potent chemical released by body cells in response to infection or allergy
Hypertension—elevated blood pressure exceeding 140/90
Hyperventilation—increased rate and/or depth of breathing leading to excessive excretion of carbon dioxide
Hypoglycemia—low blood sugar
Hypopharynx—lower portion of the pharynx (throat) at openings of trachea and esophagus
Hypotension—lower than normal blood pressure
Hypoxia—body is deprived of adequate oxygen supply
IM—intramuscular; drug administration into a muscle
Inhalation—movement of air into the lungs
Ischemic—decreased or inadequate blood supply to an organ or tissue
IV—intravenous; drug administration into a vein
Jaundice—yellow discoloration of the skin and sclera due to liver disease
Kussmaul respirations—rapid deep ventilations seen in diabetic ketoacidosis
Laryngoscope—instrument used to view the larynx
Laryngospasm—spasm (constriction) of the vocal cords
Larynx—the voice box
Magill forceps—instrument used for manipulation of structures or tubes in the pharynx
Metabolic—relating to metabolism; chemical reactions that happen within the body to maintain life
Myocardial infarction (MI)—heart attack; portion of heart muscle becomes ischemic and dies
NTG—abbreviation for nitroglycerin; blood vessel dilator
Orthopnea—difficulty breathing only when lying flat
Orthostatic hypotension—decreased blood pressure caused by rapid movements from supine to standing posture, or loss of body fluids
Osmotic—pressure on water exerted by dissolved substances in a fluid separated by a semipermeable membrane
Pallor—pale appearance to the skin due to decreased blood flow in the skin
Palpated—feeling a body part or structure
Pharynx—the throat
Pitting edema—swelling of the ankles and feet due to heart failure
PO—by mouth; administration of drugs by mouth (per os)
Polyuria—excessive urination
Post-ictal—the time period immediately following a seizure
Prodromal—initial symptom or sign
Pruritus—itching
Pulmonary edema—fluid build-up in the lung due to left heart failure
Rales—crackling or bubbling sounds heard in the chest with pulmonary edema
Respiratory rate—number of respirations per minute
Sphygmomanometer—inflatable blood pressure cuff with Velcro closure
SQ—subcutaneous; injection of drugs into subcutaneous (fat) tissue
Sternocleidomastoid—muscle of the side of the neck
Stethoscope—instrument for listening to breath or heart sounds
Stridor—high-pitched breathing sound caused by partial collapse or obstruction of the upper airway during inhalation
Supine—lying on the back in a horizontal plane; sub-supine positioning is when the head is slightly lower that the knees to return more blood flow to the brain
Syncope—fainting
Systole—contraction phase of the heart cycle
Systolic—top, or first, of the two pressures making up the blood pressure; the force of blood against the blood vessel walls during ventricular contraction
Tachycardia—a rapid heart rate, faster than 100 beats per minute
Tonic—phase of seizure where all muscles of the body remain contracted
Umbilicus—navel or belly button
Urticaria—raised wheals (hives) of the skin seen in allergic reactions
Ventricular fibrillation—disorganized heart rhythm that does not result in a pulse
Xiphoid process—lower-most pointy part of sternum
INTRODUCTION
During root canal therapy, a 68-year-old male patient becomes pale, perspires profusely, and clutches his chest. He appears confused, seizes briefly, and is now unresponsive to verbal stimuli. He is not breathing and no pulse can be felt in the carotid artery. Do you know how to handle this situation?
Medical emergencies can occur at any time in the dental office. They can happen to anyone, from the anxious patient in the reception room to the elderly diabetic who was told to skip breakfast prior to coming to her appointment. They can happen to the receptionist with a seizure disorder or to the dentist experiencing prolonged chest discomfort. In a survey of 4,000 dental offices, 75% said they had treated medical emergencies in the last ten years.1 It is estimated that the average dentist will have to deal with one or two life-threatening medical emergencies in their office during their career.2 Knowing how to handle medical emergencies will make the dental assistant more confident in his or her ability to handle all aspects of the job.
The best way to handle an emergency is to be prepared in advance.3 Whether the medical emergency occurs years in the future or this afternoon, preparation is the key. All healthcare providers should be prepared to recognize and handle medical emergencies in the office. Staff should be trained and frequently updated in first aid and cardiopulmonary resuscitation procedures. A written emergency plan should be available, and all staff members should be thoroughly familiar with it and their responsibilities in an emergency. This includes training of office personnel in handling emergencies, development and posting of office emergency guidelines, and maintenance of an emergency kit or “crash cart,” fully equipped and ready for immediate use.4
PREPARATION FOR EMERGENCIES
Most emergencies can be prevented by adequate preparation of the patient and staff. The following are suggested guidelines:
• Obtain a medical history on every patient and update it at each visit. Obtain physician consultation where necessary.
• When confirming appointments, remind patients to take their normal medications on the day of their appointment. Procedures should be scheduled around meal times for diabetics. Patients using inhalers or nitroglycerin should have these with them in the event that an asthma or angina attack is precipitated by the stress of dental treatment.
• Staff members should be trained to monitor and interpret vital signs. These should be taken at the initial visit as a “baseline reading” and at each subsequent visit for those patients whose medical history indicates they may be “at risk.”
• All staff members should be trained in basic first aid procedures and basic life support (CPR).
• The office should have a written emergency plan. Each staff member should know and practice their particular function in an emergency, and emergency telephone numbers should be posted at each phone.
• Staff members should be aware of the signs of stress and ways these can be alleviated.
• Office personnel should be aware of the signs and symptoms indicating an emergency. Each office should have an emergency kit readily available and each staff member should know where it is located.
• All staff should be aware of their legal responsibilities when responding to an office emergency.
Remember—the “best handled” medical emergency will always be the one that never happened.
HEALTH ASSESSMENT5
The increasing numbers of older patients with significant medical problems requiring dental care, longer dental appointments, and the increasing use of new medications with complex interactions all increase the risk of a life-threatening problem occurring in the dental office. The majority of medical emergencies in the dental office, however, can be anticipated and avoided with appropriate risk reduction. One key to reducing risk is to take a health history and vital signs to identify the “at risk” patient. In some cases, extensive procedures on “at risk” patients might are best performed in a hospital setting.
Health History
Prevention and preparation are often the best antidotes for an emergency. Begin by obtaining a good health history at the patient’s first visit; a sample health history form is shown in Figure 1. Other sample forms can be obtained from the American Dental Association, from dental office supply companies, the Internet, and may even be included with computer software designed for the dental office. Each office may choose to review a number of forms or develop a health history form that works best for the practice.
The health history should include information regarding the patient’s past and present health status. It should also include questions indicating problems the patient may not be aware of, but which may alter treatment. A number of medical problems that may alter dental treatment are indicated in Figure 2. The health history form should be completed in its entirety, and the assistant should obtain additional information on questions answered in the affirmative to a health concern. The completed questionnaire should then be reviewed and signed by the dentist prior to treatment.
A list of medication names and dosages currently prescribed for the patient should be ascertained. A list of common prescription medications and their usefulness is shown in Figure 3. Additional questions should be asked regarding the use of herbal or street medicines.
Every staff member who may be involved with the treatment of a particular patient should be familiar with that patient’s health history and should review it before each appointment. To keep the health history current, the patient should be questioned about any changes in their general health since their last visit. This information may be obtained while they are seated in the operatory. Figure 4 is a sample medical history update form that could be used at each appointment and then attached to the patient’s chart. The form should be signed or initialed by both the patient and the dentist.
VITAL SIGNS
Obtaining vital signs provides a baseline measurement from which alterations in the patient’s condition can be determined. This is a practice not frequently seen in dental offices. Vital signs—blood pressure, pulse, respirations, and temperature—should be measured prior to each treatment.
Temperature
Taking a temperature as part of the vitals check will often indicate if the patient has an infection. An oral temperature in excess of 99.6°F (37.5°C) is a good indicator of the presence of a viral or bacterial infection.
The other vitals—pulse, blood pressure, and respirations—can be taken while the thermometer is in the patient’s mouth, thus using little additional chairtime.
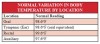
Body temperature varies with location, and may be measured where most convenient. Figure 5 lists these temperature variations by location.
In the dental office, the oral reading is most frequently used. The four most common types of thermometers include:
• Digital oral thermometer, used with plastic probe covers.
• Tympanic (ear) thermometers give a reading equivalent to the oral temperature.
• Disposable thermometer tapes.
• Standard glass thermometer with a mercury column inside, used with plastic probe covers.
Digital thermometers are popular due to their convenience and fast reading. The battery must be checked regularly for proper use and accurate readings. The digital reading is displayed on a small LCD screen after approximately 30 seconds.16
A tympanic thermometer registers the body’s temperature by bouncing an infrared signal off the eardrum. The reading is accurate and received within a few seconds. One drawback is the initial price, ranging from $40 to $100 and higher.
Disposable thermometer tapes or strips can be used orally or axially. The strips are convenient but will give inaccurate readings if improperly stored near a heat source. To receive a reading, the strip is placed in the mouth or against the forehead and the liquid crystals change color to indicate temperature.
The standard glass thermometer is the least expensive and may be calibrated in either degrees Fahrenheit or degrees Centigrade. These thermometers use mercury inside the glass cylinder to measure the temperature. Many states have banned their use because if broken, exposure to toxic mercury vapors can occur. Before taking the patient’s temperature, the mercury should be shaken down to give a reading below 95°F. Shake the thermometer with a snapping downward motion, but take care to avoid striking it against a countertop or cabinet. If a glass thermometer is accidentally broken, a mercury clean-up kit should be used to prevent contamination. For this reason many offices are choosing to use thermometers without mercury.
Whenever the temperature is taken, the reading is recorded in the patient chart on the date of service. If the temperature is significantly elevated (>100°F), circle it in red to draw the dentist’s attention to it. A typical chart entry might read: 98.6°F oral 11-5-XX
Pulse
The pulse is the pressure wave that can be felt as the heart contracts and propels a volume of blood forward in the arterial system. For routine measurement, the pulse in the radial artery in the wrist is most commonly used. Figure 6 indicates the locations of other pulse points. The radial artery can be palpated on the thumb side of the anterior aspect of the wrist. Apply gentle pressure to the artery until the pulsations can be felt. Two or three fingers should be used to assess the pulse. Avoid using your thumb; you may be feeling (and counting) your own pulse rate and not that of the patient.
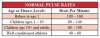
Three assessments can be made concerning the pulse: rate, strength, and regularity. The number of pulsations in 15 seconds is counted and then multiplied by 4 to obtain the pulse rate. For adults, the pulse is usually in the 60 to 100 beats-per-minute range. Normal pulse rates for other age groups are given in Figure 7. In adults, a pulse exceeding 100 beats per minute is termed tachycardia, and bradycardia if less than 60 beats per minute. Variations from this range are common. A person who exercises or runs regularly may normally have a resting heart rate less than 60, while a patient anxious about dental treatment may have a rapid pulse. Retaking the pulse in a few minutes often results in a more accurate value.
The strength of the pulse is a rough measurement of the amount of blood ejected by the heart and the amount of constriction in blood vessels. A “weak, thready (small)” pulse is an indication of shock and low blood pressure, while a “bounding (strong)” pulse is an indication of anxiety or high blood pressure. Regularity is indicated by even spacing between the beats. An irregular pulse, which indicates a rhythm disturbance of the heart, is seen in some patients and is usually not severe.
The patient’s pulse rate, strength, and regularity should be recorded on the patient’s chart, for example: 86 strong and regular.
In hypotensive or unresponsive patients, the carotid artery should be used to check for the presence of a pulse. To find the carotid artery, palpate the larynx in the midline and slide your fingers toward you into the groove formed by the border of the sternocleidomastoid muscle.
Blood Pressure
The circulatory system is a closed system. When the heart contracts, a volume of blood is propelled into the arterial system and is measured as the systolic blood pressure (systole means cardiac contraction). During relaxation of the heart, the amount of constriction (or squeeze) applied to the arteries and the volume of blood in them is measured as the diastolic pressure.
An instrument called a sphygmomanometer (blood pressure cuff) is used to measure blood pressure. The aneroid gauge (or mercury column) is calibrated in even numbers. When measuring blood pressure, it is important to select the proper cuff, as cuffs come in various sizes, including obese adult, adult, child, and infant. Cuffs that are too small for the patient may give falsely high readings. In addition, remember that cuffs should not be placed over heavy or tight clothing.
With the patient seated, and their arm resting comfortably on a level surface (the cuff should be at the same level as the heart), apply the cuff to the upper arm about one inch above the flexion crease at the elbow. Center the bladder of the cuff over the brachial artery (usually an arrow marked “artery” can be found on the cuff label). Palpate the medial aspect of the antecubital space to detect the pulsation in the brachial artery. Place the stethoscope in your ears with the earpieces pointing toward the front of your head.
Next, place the diaphragm side of the stethoscope over the spot you have located and inflate the cuff rapidly until sounds are no longer heard in the artery. Inflate the cuff 20 mmHg beyond this point, then gradually deflate the cuff while listening for “tapping” sounds in the artery. When the sounds are first heard regularly, this level is the systolic blood pressure. Note the reading on the gauge. Continue to deflate the cuff slowly. The character of the sounds will change and finally abruptly disappear; this is the diastolic blood pressure. Again, note the reading indicated on the gauge. With the test completed, fully open the valve to deflate the cuff and remove it from the patient’s arm.
The blood pressure is recorded on the patient’s chart as the systolic pressure over the diastolic pressure and also indicates the arm in which it was taken. A slight variation in blood pressure can occur between the arms; this is normal. A typical chart notation might be: 120/80 ® arm.
Blood pressure classifications are shown in Figure 8. Systolic pressures less than 20 mmHg of the patient’s normal reading may indicate hypotension. Because the diastolic pressure is the “resting” pressure of the heart, it is closely monitored for the development of hypertension. Several factors, including stress and anxiety, can raise the blood pressure and variations in blood pressure can be noted throughout the day. Before a diagnosis of hypertension is made, blood pressure should be taken on different days at different times.
Lowering blood pressure to less than 120/80 may help prevent other serious health problems as well.
Respirations
The respiratory rate is determined by the number of breaths in 6 or 15 seconds. One breath or respiratory cycle consists of one inhalation and one exhalation.
In many cases, if a patient knows someone is counting their respirations, he or she will unconsciously alter them. One easy method to measure the respiratory rate is to begin counting the rise and fall of the patient’s chest immediately after taking their blood pressure or pulse. With the stethoscope still in your ears, glance at the clock, shift your gaze toward the patient’s chest and begin counting. To obtain the respiratory rate, multiply the number of breaths in 6 seconds times 10 (or the number of breaths in 15 seconds times 4).
A normal respiratory rate for an adult at rest is between 12 and 20 times per minute. Respiratory rates for other age groups are listed in Figure 9. Factors that can increase the respiratory rate include anxiety, fever, and hypoxia. Respiratory rates can increase with age due to decreasing lung elasticity. The respiratory rate will decrease with the use of narcotics, including Demerol® and morphine, as well as with the use of the benzodiazepines such as Valium® and Versed®. Note the rate, depth, and regularity of respirations on the patient’s chart; for example, 16 normal and regular.
EMERGENCY TRAINING
Every member of the dental team should have completed a basic first aid course and have annual training in cardiopulmonary resuscitation from the American Heart Association or American Red Cross.7 The CPR course for healthcare providers is recommended because it includes two-person CPR, child and infant CPR, and the use of a mask. Although in some states CPR refresher courses are required only every 2 years, they should be taken on an annual basis. Retention studies have shown that if CPR skills are not used regularly, they are soon forgotten.
Ideally, the entire staff should take the CPR refresher course together, so they will feel comfortable working with each other if the need arises. Masks with one-way valves should be used in training and supplied to office personnel for actual patient use as specified by OSHA regulations. Bag-valve-mask devices are more difficult for the occasional user to actually ventilate a patient with such a device. Pocket masks are much easier to use, provide effective ventilations, and have ports for the addition of supplemental oxygen.
A basic first aid course provides the staff with information on emergency care in common injury situations. Topics such as the control of bleeding, treatment of burns, and the handling of sprains and fractures are covered in the course.
An automatic external defibrillator (AED) is an adjunct piece of equipment every office should consider having available as part of the office emergency kit. Some states require all dental facilities to have one, be sure to check your state law. The AED is a computerized defibrillator that recognizes the presence of ventricular fibrillation or rapid ventricular tachycardia and then allows the operator to administer “shocks” to convert the patient’s heart rhythm back to normal. For every minute that lapses before defibrillation, the survival rate decreases by 10%.17 The AED is equipped with a voice prompt to lead the operator through its usage and requires no special training.
Other more advanced emergency courses (such as those for first responders and emergency medical technicians) are available and, depending on the type of practice and location, may be advisable for the dentist and staff. Oral surgeons should be encouraged to take the Advanced Cardiac Life Support Provider course (ACLS) offered through the American Heart Association.
The 2010 AHA Guidelines for Cardiopulmonary Resuscitation (CPR) recommend a change in the Basic Life Support (BLS) sequence of steps from A-B-C (Airway, Breathing, Chest compressions) to C-A-B (Chest compressions, Airway, Breathing) for adults, children, and infants (excludes newborns). This fundamental change in the CPR sequence will require reeducation of everyone who has ever learned CPR, but the consensus of the experts is that the benefit will justify the effort.
Here is a step-by-step guide for the new CPR:
1. Call 911 or ask someone else to do so.
2. Try to get the person to respond. If he doesn’t, roll the person on his or her back.
3. Start chest compressions. Place the heel of your hand on the center of the victim’s chest. Put your other hand on top of the first with your fingers interlaced.
4. Press down so you compress the chest at least 2 inches in adults and children and 1.5 inches in infants. “One hundred times a minute or even a little faster is optimal,” Sayre says. (That’s about the same rhythm as the beat of the Bee Gee’s song “Stayin’ Alive.”)
5. If you’re been trained in CPR, you can now open the airway with a head tilt and chin lift.
6. Pinch closed the nose of the victim. Take a normal breath, cover the victim’s mouth with yours to create an airtight seal, and then give two, 1-second breaths as you watch for the chest to rise.
7. Continue compressions and breaths—30 compressions, two breaths—until help arrives.14
OFFICE EMERGENCY PLAN8
Because it is impossible to know when an emergency may occur or what form it may take, it is important that every dental office have an established, written, and practiced routine for handling emergencies.
Emergency numbers such as 911, or a 7-digit ambulance or rescue squad number in those areas without 911 services, should be posted conspicuously at every phone in the office. Other phone numbers for emergencies might include the hospital emergency department, an oral surgeon, a physician, and so forth.
A code word or phrase indicating an emergency should be determined. This will alert other staff to the existence of an emergency and avoid possible upset to patients in nearby operatories or in the reception area. The office communication system will determine the type of code to be used; four buzzes on the intercom, flashing lights, or “Page for Dr. Blue” are some examples.
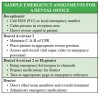
Every member of the dental staff should have a specific assignment in an emergency. To compensate for staffing variations, such as occurrences with part-time staff or during employee vacations, assignments should be doubled-up to ensure all areas are covered. The number of assignments and specific functions will be determined by staff size and training. Large offices may have several people manning an area, while smaller staffs may have multiple areas to cover. Figure 10 shows some typical emergency assignments.
The office emergency plan should be updated and practiced regularly at periodic staff meetings or following annual CPR training sessions. Mock scenarios of various emergency situations can be developed which will allow each staff member to act out their assigned roles; some samples are given in Figure 30. Later, staff members can evaluate their performance and develop modifications to the office emergency plan as needed.
Additions to the office staff should be included in the emergency plan, and their role should be covered as part of their orientation to the office. New staff should (1) review the written office emergency manual; (2) be given a specific emergency assignment; (3) be shown the location of all emergency equipment; and (4) participate in practice situations.
With careful planning and frequent practice of the office emergency plan, confusion and panic can be significantly reduced during an actual emergency.
ANXIETY REDUCTION
Stress is the major factor causing medical emergencies in the dental office. Syncope, hyperventilation, seizures, asthma attacks, and angina are some of the more common emergencies and they share one common thread—all can be precipitated by stress and anxiety.
Anxiety-related problems are fairly easy to prevent. The first step is to identify the patient likely to experience anxiety. Anxious patients tend to startle easily, have a rapid heart rate, exhibit pale and clammy skin, and appear apprehensive. In pretreatment conversations, they may relate worry about the appointment or indicate a fear of pain.
Once identified, steps can be taken to manage the anxiety proactively. A first step is to minimize the amount of waiting prior to any procedure. The procedure should be explained to the patient in a thorough and detailed manner, so that he or she experiences no surprise in the operatory. In more extreme cases, patients may need to be premedicated with anti-anxiety agents. Adequate pain control should be used and longer procedures should be divided into shorter dental appointments.
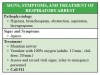
RECOGNITION OF AN EMERGENCY AND INITIAL EMERGENCY PROCEDURES
Physical signs and symptoms that may indicate an incipient medical emergency include chest pain, pale skin, sweating, vomiting, irregular respiratory rate, altered or unusual sensations, hemorrhage, and changes in pulse and blood pressure.9,10
When an emergency situation is recognized, dental treatment should be stopped immediately and assistance summoned. If the patient was receiving nitrous oxide, it should be discontinued, and 100% oxygen should be given in its place in every case but hyperventilation. Establish patient responsiveness by shaking and asking in a loud voice “Are you okay?” Lay the patient in a supine position. If the situation appears serious, call 911 immediately.
Check for the presence of a carotid pulse for 5 to 10 seconds. If no pulse is present, lay the patient flat in the chair with a board behind the chest. If this is not possible move the patient to the floor and begin chest compressions on a bared chest. Leaving the patient in the chair with a board behind the chest lessens the chance of injury that may happen by moving the patient to the floor. If the pulse is present, check the rate and strength. Begin fast chest compressions according to the new CPR guidelines. Apply the defibrillator pads of the AED as soon as it arrives, turn the unit “on” and follow the voice prompt directions. In a pulseless patient, defibrillation takes precedence over chest compressions.
Open the patient’s airway using the head-tilt chin-lift, remove any dental materials from the patient’s mouth, and suction as necessary. Assess for spontaneous breathing for 3 to 5 seconds. If the patient is not breathing, give two slow breaths via a pocket mask.
The initial emergency steps are summarized in Figure 11.
HANDLING SPECIFIC MEDICAL EMERGENCIES11
What types of emergencies can be expected in the dental office? In more than 30,000 medical emergencies reported by private practice dentists in a 10-year period, the major problem seen was syncope (fainting). The other findings of this survey are summarized in Figure 12. Over half of the problems occurred during or immediately after the administration of local anesthesia and were most commonly seen in the settings of tooth extractions or root canal therapy. This underscores the need to remain with and closely monitor patients in the operatory after administration of an anesthetic.
Airway Obstruction
Foreign bodies falling into the hypopharynx can lead to partial or complete airway obstruction. The patient may complain of a foreign body sensation in the throat, be coughing and dyspneic, exhibit stridor, or become apneic and cyanotic. They may grasp their throat with their hand (universal choking symbol) and, in the case of complete airway obstruction, will be unable to speak. If not corrected immediately, respiratory arrest will lead to cardiac arrest within minutes.
Dental materials should be eliminated as potential airway obstructions by appropriately securing the operative area.
If the patient is coughing forcefully, allow them to continue to cough, as this is their best chance for clearing their airway. If the patient is conscious, but continues to choke and is unable to breathe, abdominal thrusts should be used. Stand behind the patient, and place the thumb side of the fist into the abdomen above the umbilicus and below the rib cage. Administer slow, inward and upward thrusts until the object pops free or the patient loses consciousness.
With loss of consciousness, help the patient to the floor, open the airway, and sweep out any obstructions that can be reached with the finger. Attempt to ventilate. If the patient cannot be ventilated, the airway is still obstructed. Continue the steps for CPR—checking mouth and ventilating at the appropriate time.
With persistent airway obstruction, a laryngoscope and Magill forceps can be used to visualize the lower airway and under direct visualization, remove the obstruction.
Asthma/Bronchospasm/COPD
Asthma is an allergic response of the small airways (bronchioles). Asthma affects people of all ages, but is more common in younger people. Chronic obstructive pulmonary disease (COPD) is a mixture of emphysema and bronchitis seen in older adults. Common to both is the propensity of the small airways to spasm (bronchospasm). In patients with COPD, the retention of carbon dioxide (CO2) is a complicating factor.
In both cases, patients may respond to anxiety and aerosolized particulate matter with bronchospasm. Many cases can be prevented by pretreatment with the patient’s metered dose inhaler (puffer) of bronchodilator medication. The inhaler should also be readily available at chairside.
The patient may abruptly develop bronchospasm as evidenced by wheezing, coughing, and difficulty breathing, and may also complain of chest tightness and develop cyanosis.
The patient should be placed in an upright position with arms forward to facilitate breathing and oxygen should be administered by mask or nasal cannula. The patient should use their inhaler and self-administer one puff with instructions to inhale and exhale slowly. If the patient recovers well, treatment can continue. If the patient does not improve within 5 minutes, a second dose should be administered and it is recommended that treatment be postponed to another date.
Cardiac Arrest
Of all the emergencies that may occur in the dental office, cardiac arrest is certainly the most serious. Cardiac arrest may result from an abnormal heart rhythm or be secondary to respiratory arrest. In either case, time and immediate intervention is of the essence.
Immediately upon assessing unconsciousness in a patient, call 911. The rescuer should open the airway, look, listen, and feel for respirations. Next, check the carotid pulse for 5 to 10 seconds. If a pulse is absent, lay the patient flat with a board beneath the chest or move patient to floor. Begin the fast compressions for CPR as outlined earlier. Open the patient’s airway using the head-tilt chin-lift, remove any dental materials from the patient’s mouth, and suction as necessary. Assess for spontaneous breathing for 3 to 5 seconds. If the patient is not breathing, give two slow breaths via a pocket mask.
When possible, use the two-rescuer technique. Attach AED if available and follow the instructions. Continue to monitor all vital signs and give that information to emergency personnel when they arrive.
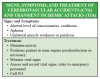
Cerebrovascular Accidents/Transient Ischemic Attacks
A cerebrovascular accident (CVA or stroke) or a transient ischemic attack (TIA) is caused by an interruption of blood flow to the brain. These episodes are usually seen in older patients as a consequence of atherosclerosis or untreated hypertension. The interruption in flow may be due to a blood clot, spasm of the arteries, or even to rupture of a blood vessel in the brain. Blood flow to the cerebral cortex is insufficient and the patient will exhibit symptoms within seconds. The signs and symptoms may be of short duration (TIA) that resolve spontaneously or persist for months or years. A transient ischemic attack is a forewarning of a major ischemic CVA, and a physician must evaluate these patients to prevent such an occurrence.
F.A.S.T. signs can be used quickly to determine if a patient may be experiencing a CVA. The patient may have an altered level of consciousness or periods of confusion. Weakness or paralysis in one half of the body (right or left side) may be obvious. The patient may also be unable to speak or understand speech. When these severe symptoms occur without warning, they are likely to alarm both the patient and staff.
When faced with a TIA or CVA, 911 should be called immediately. Place the patient on their side to maintain their airway, and suction oral secretions to prevent aspiration. These are both necessary as the patient frequently loses control of the facial muscles. Calm and reassure the patient and monitor their vital signs. Oxygen may also be administered if the patient is having trouble breathing.
If an ischemic stroke is confirmed, and the onset of symptoms has been less than 3 hours, a medication will be administered to help remove the clot and restore blood flow to the affected brain areas.
Chest Pain/Angina/Acute Myocardial Infarction
The development of central chest discomfort frequently results from stressful situations in patients with coronary artery disease. In angina episodes, the coronary artery narrowed by atherosclerosis is unable to supply the heart muscle with adequate amounts of oxygenated blood, causing chest pain. The onset of anginal chest pain is usually directly related to exercise, stress, and anxiety. The decreased oxygen supply to the heart muscle is usually of short duration (less than 5 minutes) and no permanent damage occurs.
In myocardial infarction (MI or heart attack), a blood clot develops in one of the coronary arteries completely cutting off blood supply to a portion of the heart muscle. Without a blood supply, the heart muscle dies within a few hours. The ischemic heart is very irritable and susceptible to cardiac arrhythmias. This is the patient most susceptible to sudden death. Whenever and wherever a myocardial infarction is recognized, 911 must be called immediately. This is critical, as about 50% of patients experiencing a myocardial infarction will die in the first two hours.
In both cases the patient will complain of chest pain usually described as a pressure or weighty sensation. This pain or numbness may radiate into either of their shoulders, arm, the neck, jaw, straight through to the back or to the upper part of the abdomen. Complaints of shortness of breath, nausea, or vomiting are common, and the patient’s skin may be pale and sweaty. If the patient has experienced angina in the past, they will be able to determine if this pain is different in character.
Place the patient in whatever position is most comfortable. It is recommended that out-of-hospital patients are administered a single, chewed dose of 162 mg to 325 mg of aspirin to begin fibrinolysis. When chewed, the clinical effects are realized more quickly. Administer oxygen and monitor vital signs. Nitroglycerin 0.4 mg may be administered sublingually every 5 minutes but is usually more effective in treating the pain associated with an angina episode. If the patient has not previously had nitroglycerin, it is advisable to administer it while the patient is in a supine position, as hypotension is frequently seen in first-time users. Calm and reassure the patient. The experience can be extremely frightening, with some patients voicing feelings of impending doom or death.
Heart Failure/Pulmonary Edema
Heart failure results when one of the ventricles is unable to completely pump all of the blood filling the chamber forward into the arteries. Heart failure may involve either the left ventricle (left ventricular failure, LVF) or the right ventricle (right ventricular failure, RVF). Of the two, left ventricular failure is the more serious and occurs first. In LVF, blood backs up into the lungs causing pulmonary congestion and shortness of breath, particularly when the patient is lying flat. In RVF, the blood backs up into peripheral circulation causing swollen legs and ankles resulting in pitting edema.
Left ventricular failure is frequently precipitated by an acute myocardial infarction. When this occurs, call the rescue squad (911) immediately and place the patient in whatever position is most comfortable for them, usually sitting bolt upright. Administer oxygen by mask and monitor vital signs. If the patient complains of chest pain, nitroglycerin may be given.
Hypoglycemia
Hypoglycemia occurs when there is insufficient glucose in the bloodstream to meet the metabolic demands of cells. True hypoglycemia is seen only in insulin dependent diabetics (Type 1) or in Type 2 diabetics using oral hypoglycemic agents such as Diabeta®, Orinase®, or Glucotrol®. The lack of glucose in the neurons of the central nervous system results in immediate dysfunction, causing the patient to appear confused and restless. Patients may also complain of a headache or exhibit bizarre behavior. Their skin becomes pale, cool and clammy, and their heart rate increases. On occasion, a patient may exhibit seizure activity or transient stroke-like symptoms. If a source of glucose is not administered immediately, permanent damage may result.
Hypoglycemia occurs when blood sugar levels drop below 80 mg/dl and typically becomes more acute in the 20-mg/dl to 30 mg/dl range.
Hypoglycemia can be prevented by making sure the insulin dependent diabetic has eaten before treatment, by scheduling appointments in the morning, and by having a glucose source readily available at chairside. If the patient exhibits signs and symptoms of hypoglycemia, administer an oral carbohydrate such as regular cola, table sugar, or even a spoonful of honey or icing to raise blood glucose levels. For a patient who becomes unconscious, maintain their airway, turn the patient on their side to prevent aspiration and administer glucose in the dependent cheek. This will usually provide sufficient glucose to allow the patient to regain consciousness. The patient should then drink a liquid high in sugar to increase their blood glucose level. Following a hypoglycemic reaction, advise the patient to eat a meal to maintain blood sugar levels and prevent a recurrence of the hypoglycemic episode.
Diabetic Ketoacidosis
Diabetic ketoacidosis occurs when there is not enough insulin available to move glucose into cells. This causes the cells to use fats and proteins for energy, leaving behind waste products that build up in the blood. Over time, from hours to days to sometimes weeks, the blood sugar level continually increases. Frequently an underlying medical problem such as heart attack, infection, or stroke may precipitate diabetic ketoacidosis even in diabetics who are normally in good control.
The signs and symptoms of diabetic ketoacidosis are related to the osmotic effects of the very high blood sugar, the cellular acidosis, and the body’s attempt to compensate for the acidosis. Patients may hyperventilate and have a fruity odor to their breath; extreme thirst due to severe dehydration and polyuria are also common. Because of the loss of fluids, the skin is warm, red, and dry to the touch. As the dehydration and acidosis become more severe, blood sugar levels will exceed 300 mg/dl, and the patient finally may lose consciousness.
Maintain airway and ventilations by placing the patient on their side to prevent aspiration. Treatment of hyperglycemia will require hospitalization of the patient.
Allergy/Anaphylaxis
An allergic reaction is the result of an antigen-antibody reaction to a substance to which the patient has been previously sensitized. Histamine and other complex chemicals are released from body cells causing symptoms in the patient. These symptoms may be confined to a single organ system or become generalized (anaphylaxis).
In the dental office, the most likely culprits are exposures to latex, local anesthetics, or antibiotics, but foods the patient may have eaten prior to their visit such as nuts, shellfish, milk products, and strawberries can also trigger this syndrome.
The allergic reaction is frequently seen only in the body system that first came into contact with the allergen. Wheezing may be the result of something the patient may have inhaled which affects the lungs. A reaction may also be due to an injection of local anesthetic or antibiotic, resulting in a skin rash with intense itching. In other cases, ingested foods may lead to swelling of the upper airway and stridor. In its most severe form, an allergic reaction can progress to anaphylaxis, a condition in which several body systems are affected simultaneously.
The treatment of allergic reactions and anaphylaxis is the same-provide supportive care and administer epinephrine. Maintain the patient’s airway, administer oxygen, and monitor the vital signs. Administer epinephrine 1:1000 0.3 mg to 0.5 mg SQ, often into the upper arm or thigh. Every office should include at least three auto-injector epinephrine pens in their office emergency kit. Twinject® and Epi-Pen® are the most common pens for kits. Epinephrine is the treatment of choice for allergic reactions, as it reverses all the histamine-induced symptoms and blocks the further release of histamine. Benadryl® 50 mg IM or PO may be administered to treat the hives and relieve itching of the skin. Call 911 immediately as anaphylaxis may be a life-threatening emergency.
Accidental Overdose
Rapid administration, excessive dosing, or inadvertent intravascular administration may all result in increased drug effects. Prevention is the key in avoiding adverse drug reactions. Question the patient before treatment about allergies and hypersensitivity.
If the drug is to be injected IV, administer it slowly, and use the minimum amount required to achieve the desired effect. When administering blocks, use an aspirating syringe. A child’s body size and weight should be considered during dosing and anesthetic administration.
Most drugs have a few specific antidotes available. There are two notable exceptions. Narcan® (naloxone) is the antidote for accidental overdose of narcotics given IV such as Demerol® (meperidine).
Narcan® can be used to reverse the hypotension, respiratory depression, and decreased level of consciousness caused by these narcotics. In the case of the benzodiazepines such as Valium® (diazepam) and Versed® (midazolam), a specific antidote—Romazicon® (flumazenil) —is also available.
The patient should be treated supportively until the effects of the drug wear off. Stop the administration of the drug, maintain the airway and ventilations, monitor vital signs, and contact 911 if the patient fails to show prompt improvement.
All of the toxic effects of lidocaine are due to its effects on the central nervous system and the conduction of nerve impulses. The signs and symptoms of lidocaine toxicity are shown in Figure 22. As there is no specific antidote for lidocaine toxicity, provide supportive care. Maintain the airway, administer oxygen, and treat other problems as they arise.
Hyperventilation Syndrome
Anxiety, fear, and pain in susceptible individuals can result in a conscious overdrive of ventilation called hyperventilation. The excessive excretion of carbon dioxide that occurs due to the greatly increased respiratory rate can cause unpleasant symptoms that exacerbate the situation. Apprehension and air hunger (a sense that they “can’t catch their breath”) coupled with numbness and tingling in the arms and legs give the patient the sensation (although erroneous) that something is seriously wrong. The hyperventilation may progress to the point where the patient develops painful carpopedal spasm and may even have a syncopal episode. As soon as the patient faints, however, the respiratory rate immediately returns to normal.
Hyperventilation is the only emergency when oxygen administration is not called for in the treatment plan. The old treatment which involved use of a paper bag should be avoided, as it may increase carbon dioxide to dangerously high levels in patients with a metabolic cause for their hyperventilation, such as diabetic ketoacidosis. Instead, make the patient aware of how fast they are breathing and assure them that all of their symptoms are related to their fast respiratory rate. Coach the patient to take slow, regular breaths on a breath-by-breath basis. If necessary, use a detached oxygen mask that has holes for the release of excessive carbon dioxide to help reassure and calm the patient.
Respiratory Arrest
The end result of bronchospasm, hypoxia, airway obstruction, aspiration, and laryngospasm may be respiratory arrest. Patients who stop breathing will be unresponsive. Instruct someone to call 911 immediately. Open the patient’s airway, and look, listen, and feel for airflow over the mouth and nose. If the patient is not breathing, place a pocket mask over the patient’s mouth and nose, maintain the head tilt, and deliver a slow ventilation until the patient’s chest rises. Repeat this ventilation and check the patient’s pulse. If the pulse is present, ventilate an adult 12 times per minute (one breath every 5 seconds); for children or infants, ventilate 20 times per minute (one breath every 3 seconds). Be careful to ventilate only until the patient’s chest rises, as overventilation will distend the stomach with air and cause vomiting. Continue ventilations with periodic checks of the pulse until the rescue squad arrives.
Seizures
Convulsions or seizures are caused by waves of abnormal electrical activity in the brain. As these waves spread across the surface of the brain, they stimulate other cells that are responsible for motor activity, sensation, or consciousness.
Seizures are most commonly seen in patients with known seizure disorders such as epilepsy. Such patients may have stopped taking or missed a dose of their anti-seizure medication or they may experience a seizure as a result of exposure to a triggered or stressful situation. It is important to note that otherwise “normal” patients may seize if the conditions are right, particularly with hypoglycemia or hypoxia.
In some cases, the patient may have a premonition they are about to have a seizure. This premonition, called an aura, may take the form of a strange smell, visual or auditory hallucination, or other strange sensation. This allows the patient some time—ranging from a few seconds to minutes—to prepare for the seizure. As a seizure begins, the patient typically loses consciousness and then becomes tonic as all of the major skeletal muscles contract. The patient is then apneic, becomes cyanotic, and may bite their tongue. This is followed by the clonic phase in which muscles contract and relax in waves. During this phase, these involuntary movements make the patient susceptible to injuries to the head, arms, or legs, and they may become incontinent of urine and stool. A seizure is followed by a period of drowsiness, confusion, and extreme fatigue called the postictal phase.
When observing a generalized motor seizure, knowing what not to do is as important as knowing what to do. Never attempt to place or force any object between the patient’s teeth. Bite sticks are ineffective and may cause damage to oral structures. Do not attempt to restrain the patient’s movements. Individuals experiencing a seizure exhibit incredible strength and attempts at restraint may result in fractures to the patient’s bones. In addition, do not attempt to ventilate the patient during a seizure.
Loosen any constrictive clothing and turn the patient on their side to protect their airway from vomiting and aspiration. Place padding beneath the patient’s head to prevent injury and let the seizure run its course. While seizures invariably last only 1 to 2 minutes, the time seems much longer as the event is being witnessed. After the seizure, continue to monitor the airway, administer oxygen, and obtain vital signs.
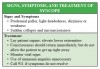
Syncope
Fainting or syncope results from either the psychological response to fear, anxiety, stress, pain, or unpleasant situations or from poor autonomic adjustments to changes in the patient’s posture. In some cases, syncope may be due to very rapid or slow cardiac arrhythmias. Syncope accounts for more than 50% of reported emergencies in the dental office.
The psychological reaction causes an abrupt slowing of the heart rate and pooling of blood in the extremities. Within seconds the patient may complain of a flushed sensation, followed rapidly by loss of consciousness.
Syncope can be prevented by identifying the patient who is prone to anxiety or who is using anti-anxiety agents. Fearful patients can be prescribed a premedication to help them relax for the dental visit. Keep the patient supine if possible; with older patients, allow them time to slowly adjust to an upright posture after procedures are completed. In the elderly, rapid changes in posture can result in postural (orthostatic) hypotension.
When faced with a fainting episode, help the patient to the floor or place them in a supine position in the dental chair with the legs elevated. Once supine, the patient will regain consciousness almost immediately. Administer oxygen and loosen any tight clothing. Do not allow the patient to sit up, as they will frequently faint again. Keep the patient supine for a few minutes while the team attempts to determine the cause of the episode. Monitor vital signs. Because the patient regains consciousness almost immediately, the use of ammonia inhalants is unnecessary. It is recommended that treatment be stopped and rescheduled for another date.
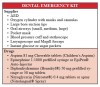
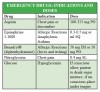
EMERGENCY KIT
Every dental office should have an emergency kit.12 Commercially available kits are expensive and contain drugs and equipment that will never be used; in fact, some of these kits contain drugs that have not been used in general medicine for 20 years. A kit can very easily—and inexpensively—be assembled, although the actual drugs in the kit should be selected by the dentist. Never include drugs or equipment that the dentist is not trained to use or comfortable in administering. Drugs can be purchased from a hospital pharmacy and the other supplies obtained from a local medical equipment company. Figure 27 lists the suggested contents of an emergency kit for the dental office.
Another general rule to kit supplies relates to how close the office is to emergency help. Rural offices may need to have more medicines in their kit to administer until help can arrive. Urban and suburban offices may be able to just have the basic supplies because help will reach them more quickly.
All of the materials (except the oxygen cylinder and AED) can be stored in a large tackle box for portability. The kit should be kept in a prominent, easily accessible location known to everyone in the office. Someone on the dental team should be responsible to periodically check all items to ensure that none of the drugs have passed their expiration date and all equipment is operational.
A card that clearly states the indication, dosage, and administration of the drugs in the kit should be taped inside the lid. In an emergency situation, infrequently used doses can easily be forgotten. Each of the drugs listed is available in prefilled syringes so that no time will be lost drawing drugs up in syringes. A sample emergency drug card is shown in Figure 28. The drugs in the kit should be kept simple, as their purpose is only to handle life-threatening problems until the rescue squad arrives.
EMERGENCY TREATMENT RECORDS AND EVALUATION
A record of an office emergency should be included in the patient’s records. When an emergency occurs in the office be sure to note all details in the patient’s chart. A sample emergency treatment form is shown in Figure 29.
Following the emergency event, a post-emergency assessment of the situation should be done with all those involved evaluating each other’s performance. In this way, problems can be identified and corrections made to the office emergency plan as required.
When reviewing the emergency, the first part of the evaluation should consider the situation and address the following:
• How early was the emergency detected?
• Did the patient’s history or chart indicate a problem might occur?
• Were any warning stickers or alerts messages posted within the patient’s record?
• What preventive measures might have been taken?
• Were treatment recommendations followed?
• What could be done next time to avoid the situation?
The second part of the evaluation looks at the performance of the “team.”
• How did the office staff respond?
• Did staff members complete their assignments efficiently or was there panic and confusion?
• Did any members of the team experience difficulties?
• Was the staff emotionally prepared to handle the emergency?
• Do the role assignments need to be modified?
The final part of the evaluation considers equipment and supplies.
• Was the equipment (emergency kit/cart) stored in the designated location?
• Was all equipment present and functional?
• Were drugs unexpired and correctly prepared?
• If CPR was performed, did the team follow the most recent accepted protocols?
The main goal of the evaluation is to define strategies to either avoid a crisis or if unforeseeable to provide appropriate patient care.
LEGAL ASPECTS13
The legal obligations in the dental office rest principally with the dentist. However, assistants must be aware of state dental practice acts and any rulings that could involve the assistant. In many states current CPR status for auxiliaries is required. Always remember: ignorance of the law does not constitute immunity from liability.
In addition to familiarity with state dental practice acts, the dentist should also be aware of accepted treatments and protocols for medical emergencies which often become the basis for a legal standard of care. The standard of care can be defined as “what the reasonable, prudent person with the same level of training and experience would have done in the same or similar circumstances.”
The first component is a duty to act. There is no doubt that a healthcare provider is required to render necessary emergency care to an individual in an office, whether that individual is a patient, family member, or an employee. The expectation of the general public is that they are in a healthcare facility and that its employees should be trained for such emergencies.
The second part is an act of omission or commission. An act of omission would be failing to carry out some task that the “reasonable, prudent person” would have performed under the circumstances. An act of commission would be an attempt to provide care beyond what was normally accepted under the circumstances or by failing to have taken an action that would have prevented an emergency.
The third point that would have to be proven is that the patient was actually injured in some way. In most cases, this would be some type of physical injury, but it could also include emotional or economic damages.
The fourth point—that the assistant’s failure to act as a reasonable, prudent person was the proximate cause of the patient’s injuries—ties everything together.
This cycle of potential malpractice can be avoided by safeguarding the patient’s interests, performing as expected in an emergency, and acting within the scope of your practice.
Taking into consideration these legal aspects concerning emergency treatment, always keep in mind the following points:
1. When an emergency arises, call for EMS (911) immediately. There are cases on record in which dentists have been sued for not calling an ambulance in a timely manner. In handling an office emergency, the goal should always be to maintain the patient and provide appropriate treatment until the rescue squad arrives. Rescue squad personnel will not mind if they arrive at the scene only to find a patient not requiring further treatment or transport. Once the rescue squad arrives, however, they and their medical control physician (via radio) are in charge of the patient’s medical treatment.
2. If there is a problem, such as a dental dam clamp falling into a patient’s throat, be honest with patients as to the nature of the problem.
3. Refer patients to medical professionals when necessary. Never attempt to treat situations that require physician or hospital management.
4. Be knowledgeable about state dental practice acts and your requirements for dealing with emergencies.
5. Take a complete health history for new patients and update it at each visit. Maintain adequate records. Document emergency treatment rendered; generally, courts have maintained that if it wasn’t written down, it wasn’t done.
6. Take vital signs, especially if an anesthetic is to be administered.
7. Having an emergency kit in the office does not prevent liability unless you know how to use it properly.
SUMMARY
It has been estimated that one or two life-threatening emergencies will occur in the lifetime practice of a general dentist. With the aging of the population generally and the more frequent appearance in the dental office of individuals with underlying medical conditions, the possibility of problems occurring will only increase. Obtaining a health history and a set of vital signs is the first step in identifying the patient likely to develop a medical emergency. With proper training, thorough preparation, and regular practice, the staff of the dental office will be able to provide appropriate medical care should the need arise.
ABOUT THE AUTHORS
Sue Protzman, was a certified dental assistant in a variety of office settings for over 35 years and was affiliated with the dental assisting program at Northeast Wisconsin Technical College in Green Bay, Wisconsin, for 30 years. An instructor trainer in Basic Cardiac Life Support through the American Heart Association, she taught CPR and emergency aid courses at NWTC. Sue was president of the ADAA in 1989–1990 and is now retired.
Jeff Clark, MS, REMT-P, has been the coordinator and instructor of advanced emergency medical services at Northeast Wisconsin Technical College in Green Bay, Wisconsin, for more than 30 years. While primarily specializing in paramedic education, he pioneered a course in medical emergencies in the dental office for practicing dentists. As a member of the Advanced Cardiac Life Support Affiliate Faculty for the American Heart Association, one focus of his career has been reducing premature death from cardiovascular disease through instruction at both the Basic Cardiac Life Support (BCLS) and the Advanced Cardiac Life Support (ACLS) levels.
Wilhemina Leeuw, MS, CDA, is a clinical assistant professor of dental education at Indiana University Purdue University, Fort Wayne. A DANB Certified Dental Assistant since 1985, she worked in private practice for more than 12 years before beginning her teaching career in the dental assisting program at IPFW. She is very active in her local and Indiana state dental assisting organizations. Her educational background includes dental assisting—both clinical and office management—and she received her Master of Science degree in organizational leadership and supervision. She is also the continuing education coordinator for the American Dental Assistants Association.
REFERENCES
1. Being prepared for office emergencies. The Dental Assistant Update. 1994;3(3):3,8.
2. Theisen FC, Feil PH, Schultz R. Self perceptions of skill in office medical emergencies. J Dental Educ. 1990;54(10):623-625.
3. Fast TB, Martin MD, Ellis TM. Emergency preparedness: A survey of dental practitioners. J Am Dent Assoc. 1986;112:499-500.
4. Braun RJ. The dental assistant’s role in medical emergencies. The Dental Assistant. 1985;Sept/Oct:19-22.
5. Alty CT. Coping with a medical crisis. RDH. 2002;Aug.
6. Wahl MJ. Myths of dental-induced endocarditis. Arch Intern Med. 1994;154(2):137-144.
7. Bertold M. Florida mandates defibrillators in dental offices. http://www.ada.org/prof/resources/ pubs/adanews/adanewsarticle.asp?articlesid=1371. Accessed February 2006.
8. Anderson PE. Effectively handling medical emergencies. Dental Econ. 1989(Nov):54-61.
9. Curriculum guidelines for management of medical emergencies in dental education. J Dent Educ. 1990;54(6):337-338.
10. Curricular guidelines for management of medical emergencies in dental education. J Dent Educ. 1981;45(6):379-381.
11. Malamed SF. Managing medical emergencies. J Am Dent Assoc. 1993;124:40-51.
12. Weissman D. Emergency education. J Am Dent Assoc, 1993;124:51-53.
13. Wakeen LM. Dental office emergencies: Do you know your legal obligations? J Am Dent Assoc. 1993;124:54-57.
14. Highlights of the 2010 American Heart Association CPR Guidelines. http://www.heart.org/idc/groups/heart-public/@wcm/@ecc/documents/downloadable/ucm_317350.pdf. Accessed March 9, 2011.
15. Grimes E. Medical Emergencies: Essentials for the Dental Professional. Pearson Education, Upper Saddle River, NJ. 2009.
16. Bird D, Robinson D. Modern Dental Assisting, Ninth Edition. Elsevier, St. Louis, MO. 2009.
17. Malamed S. Emergency medicine. Dental Econ. 2010;(Feb):38-43.
18. Wall HK, Beagan BM, O’Neill HJ, et al. Addressing stroke signs and symptoms through public education: the Stroke Heroes Act FAST campaign. Prev Chronic Dis. 2008;5(2). http://www.cdc.gov/pcd/issues/2008/apr/07_0214.htm. Accessed April 20, 2011.
SUGGESTED READINGS
Chernega JB. Emergency Guide for Dental Auxiliaries. 3rd ed. Delmar Publishers Inc, Albany, NY, 2001.
Haas DA. Emergency supplement J Am Dent Assoc. 2010;141;8-13.
Pollack AN. Emergency Care and Transportation of the Sick and Injured. 10th ed. 2010; American Academy of Orthopedic Surgeons, Rosemont, IL.
Limmer D, O’Keefe MF. Emergency Care. 11th ed. 2008; Prentice Hall Higher Education, Upper Saddle River, NJ.
Little JW, Falace DA. Dental Management of the Medically Compromised Patient. 7th ed. 2007; St. Louis: Mosby-Year Book, Inc.
Malamed SF. Medical Emergencies in the Dental Office. 6th ed. 2007; St. Louis: Mosby-Year Book, Inc.
Meiller T, et al. Dental Office Medical Emergencies: A Manual of Office Response Protocols. 4th ed. 2010; Lexi-Comp Company.
Secrest BG. Detecting, evaluating and treating hypertension. J Am Dent Assoc. 1994;125:104-106.