You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
The ADAA has an obligation to disseminate knowledge in the field of dentistry. Sponsorship of a continuing education program by the ADAA does not necessarily imply endorsement of a particular philosophy, product, or technique.
By law and by practice, the dentist is responsible for diagnosing conditions of the teeth and jaws. Nevertheless, the whole team of dental professionals should have knowledge of how basic dental diseases appear on radiographic images. This knowledge will help the auxiliary to understand the importance of high-quality, diagnostic radiographic images and will, in the long run, make him or her that much more valuable to the dental team.
Defective Restorations and Dental Caries
Defective Restorations
The junction of a restored tooth and the restorative material should always appear sharp and distinct, though there will be some qualitative differences for interposed radiolucent bases. Restorations that radiographically fail to extend to tooth preparation margins (open margins), those that extend beyond the preparation margins (overhangs), and those with inappropriate contours may be considered defective restorations. Such restorations are usually defective at the time they are inserted, though they may become defective as a result of fracture, attrition, abrasion or erosion.
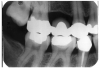
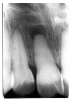
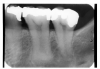
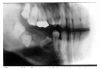
Figure 1 is a molar bitewing radiographic image that discloses a defective abutment restoration on tooth #4. The restoration ends short leaving open margins.
Enamel Caries
While advanced dental caries may well involve the entire tooth, early or incipient caries involves only the enamel. Once a carious lesion penetrates through the enamel, it is usually considered to be dentinal caries. Clinically, enamel caries usually appears as a stained system of occlusal grooves or as chalky white bands along the labial/buccal gingival aspects of the teeth. Radiographically, enamel caries is characterized by a focal loss of the normal enamel radiopacity, particularly on the interproximal surfaces.
It appears as a radiolucent cone shape, with the base at the exterior surface and the tip of the cone toward the pulp. The lesion follows the enamel rods. After progression into the dentin the lesion usually takes on a radiolucent fan shape.
To locate interproximal caries, an interproximal or bitewing survey is usually most valuable because the maxillary and mandibular teeth are simultaneously imaged on one image and the projection geometry is most favorable for accurate imaging. Anterior bitewing examination requires a change of geometry, which is not as favorable for interproximal caries detection. These interproximal surfaces are thin and can be easily examined clinically. Periapical examination of the anterior region is useful for the detection of cemental caries.
To be detectable on a radiographic image there must be a 30% to 50% change in the mineral content of the enamel lesion. Less than 30% demineralization will not produce a detectable image. The advancing edge of the lesion may not be 30% demineralized and thus will appear smaller in the radiographic image because the rest of the advancing edge is not radiographically visible. Clinically the lesion will usually be larger than its radiographic image.
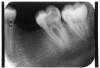
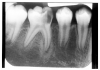
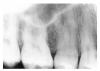
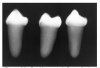
Figure 2 illustrates advanced enamel caries on the mesial surface of the premolar.
Dentin Caries
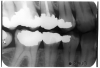
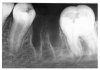
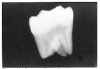
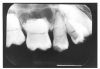
Dentin caries extends into the tooth dentin and can be recognized by noting the focal loss of dentinal radiopacity. Most commonly, this darkened dentin is located beneath carious enamel and, typically, the lateral dimension of the dentinal involvement exceeds that of the associated enamel caries (Figure 3). Dentin caries may be discerned interproximally, on the occlusal surface, buccally/lingually, or on root surfaces.
Incipient occlusal dentin caries may be difficult to identify on radiographic images and root caries must be carefully distinguished from cervical burnout, as we will discuss later.
Recurrent Caries
Recurrent caries is the condition in which carious lesions develop or extend along the margins of existing restorations. A diligent search for recurrent caries should be made whenever radiographic images detect:
• interproximal restoration overhangs
• open margins on restorations
• restorations which appear to end short of preparation margins; or
• restorations which appear unusually shallow as judged by the thickness of the restorative material.
Radiographically, recurrent caries presents as radiolucent lines that extend inward from the tooth surface along a restoration or as radiolucent zones, which appear to lie completely beneath the restoration without any observable communication with the tooth surface. As mentioned previously, the junction of a restored tooth and the restorative material should appear sharp and distinct, and, as a rule, recurrent caries should be suspected whenever radiolucencies are present between the tooth and the restoration.
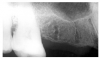
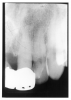
In Figure 4, recurrent caries appears at the mesial of tooth #3 and #4, and the distal of tooth #28. Also, note areas of interproximal caries on teeth #5-6.
Cervical Burnout and Mach Banding
Cervical burnout is an area of apparently increased radiolucency in the mesial and distal cervical (neck) regions of the tooth. Such regions are often mistaken for interproximal caries when in fact they only appear radiolucent because they have neither the radiopaque enamel of the region immediately above nor the bone tissue below.
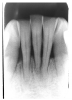
Figure 5 illustrates cervical burnout in a premolar bitewing radiographic image. Note that the cementoenamel junction and the crest of the alveolar bone lie respectively just above and just below the burnout area. As a point of comparison, note the interproximal enamel caries on the first and second premolars.
While carious lesions and areas of cervical burnout do resemble each other, there are a couple of tips to help differentiate between them. First, cervical burnout is found only in the cervical region or tooth neck, which is fortunately an uncommon area for caries to develop. Second, the cementoenamel junctions sharply limit areas of burnout incisally and occlusally, as the alveolar crest limits the area apically. Caries would not be so sharply defined.
Occlusal caries may be undetectable on a radiographic image until the decay reaches the dentin. Early radiographic appearance may be a thin radiolucent shadow below the enamel. An optical illusion referred to as Mach banding can produce the same image in healthy teeth. Detection of incipient occlusal caries is most effective by direct clinical examination.
Periodontal Disease
A tooth in the intact periodontium maintains firm attachment to a collar of the gingiva through connective tissue fibers. Beneath the gingiva, bone is attached to the root surface through the periodontal ligament, a complex system of fibrous connective tissue. Deposits of free bacteria and bacteria-rich plaque produce inflammation in the gingival collar, which, in turn, disrupts the fibrous gingival-tooth attachment.
The continued presence of plaque and calculus produces inflammation in the periodontal ligament, leading to bone loss and weakened attachment strength between the ligament and the tooth. In time, the inflammatory process can cause considerable bone loss – to the point that the tooth becomes unstable and eventually is lost.
Ongoing research is pointing towards collaboration between certain systemic diseases and periodontal health. As dental professionals it is our responsibility to discuss these findings with our patients.
Clinically, the extensive bone loss and gingival recession of advanced periodontal disease may be easily visualized. In less advanced cases, the periodontal probe can be used to measure the distance between the gingival crest and the periodontal attachment. Bleeding at the point of probing and measurement of significant distances are strong indications of periodontal disease. Figure 6 radiographically illustrates probe depth in a case of moderate periodontal disease with early alveolar bone loss.
Figure 7 illustrates severe periodontal disease with extensive loss of alveolar bone around the tooth.
Dental Calculus
Dental Calculus is mineralized dental plaque. Heavy calculus deposits are most commonly found opposite the salivary duct orifices located near the mandibular incisors and maxillary molars. Calculus is usually classified as supragingival, which occurs above the gingiva on the exposed tooth surfaces and subgingival, which is found beneath the gingiva. It is well known that the bacteria on the calculus induces inflammation in the periodontal tissue and contributes to the development of gingivitis and periodontal disease.
On a dental radiographic image, calculus is commonly seen interproximally, either filling the dental embrasures or producing distinct radiopaque spurs such as that seen on the distal of the maxillary molar in Figure 8.
At times, calculus deposits become so heavy that they completely surround the tooth. Not surprisingly, such severe cases are associated with advance periodontal bone loss.
Proliferative Gingival Hyperplasia
Gingival enlargements arise from a variety of local and systemic factors, and may be localized (Figure 9) or may involve the entire gingival area. Localized gingival enlargements most commonly result when a discrete area of the gingiva is irritated by plaque, calculus or extrinsic factors such as popcorn hulls or hard candy. Less frequently, local conditions represent an extension of underlying bone disease.
Generalized gingival enlargement may result from longstanding, chronic inflammation such as that noted in chronic gingivitis or periodontitis. It has also been associated with the hormonal changes that occur with puberty and pregnancy, with certain drug therapy (i.e., cyclosporins, dilantin, nifedipine), with systemic disorders such as scurvy and leukemia, and with genetic disorders such as fibromatosis gingiva.
In nearly all cases, generalized gingival enlargements produce only minimal osseous change; and, thus, if they are definable on radiographic images at all, it is only on the basis of their increased gingival soft tissue outline.
Horizontal Bone Loss
Generalized, extensive periodontal bone loss, in which the crest of the residual bone is parallel to the cementoenamel junction, is referred to as horizontal bone loss (Figure 10).
Vertical Bone Loss
With periodontal disease, bone loss may be relatively severe around some teeth, while leaving the immediately adjacent teeth firmly anchored. Such focal loss creates osseous defects whose height varies markedly compared to the adjacent tooth crowns. This defect is known as vertical bone loss and can be recognized on a radiographic image by noting that a line representing the residual bone crest sharply intersects another line between the tooth necks. Vertical loss is sharply apparent distal to the maxillary first molar and between the premolars in Figure 11.
Vertical bone loss may extend to the root apex, and prominent calculus deposits are often noted. Care must be taken to assess the degree of bone loss, especially around molars where special attention should be directed to the furcational periodontal ligament space.
Vertical bone loss extending into this area may appear as a focally widened ligament space.
Periapical Pathology
Acute Apical Periodontitis
Following the necrosis of the dental pulp through any cause, irritants drain and can cause a reaction in the periodontal tissues adjacent to the apical foramen. There is usually little, if any, immediate bone resorption, therefore apical periodontitis is often difficult to detect with radiographic images except that the tooth may appear slightly elevated in the tooth socket due to the collection of inflammatory exudate.
Acute Periapical Abscess
Acute, by definition, means short term. Acute abscesses often show little radiographic change because over the short run, the body has not had sufficient time to resorb bone.
Chronic Periapical Abscess
The chronic periapical abscess represents a suppurative process that has been present long enough to cause the body to resorb bone. It is not possible to absolutely differentiate between a chronic abscess, dental granuloma, or small radicular cyst solely by using a dental radiographic image. However, a radiographic image of multiple foraminae (many openings or passages) within the pathological area is strongly suggestive of sinus tract formation and drainage of pus. Notice the four prominently radiolucent foraminae in the resorbed periapical area in Figure 12.
Periapical Granuloma
The periapical granuloma represents the body’s defense mechanism attempting to wall off irritants draining from a non-vital dental pulp. While they cannot be radiologically differentiated from abscesses or cysts, they can be differentiated from normal anatomical landmarks such as the incisive fossa because the periodontal ligament space is widened and the lamina dura is not continuously intact.
Figure 13 illustrates apical periodontal pathosis in the area of the right central incisor. Note the loss of continuity of the lamina dura and the widened periodontal ligament space on the affected side.
Apical Radicular Cyst
Epithelial remnants from tooth formation are always present as builder’s debris within the periodontium. These remnants can proliferate within an apical granuloma to form an apical radicular cyst, which can grow to several centimeters if left untreated. Apical radiolucencies greater than about six millimeters usually contain epithelial cyst material. Figure 14 illustrates a clearly defined apical periodontal cyst in a pulpless tooth following acute trauma.
If the process starts from a lateral, rather than an apical canal, a lateral radicular cyst can occur. Notice how the cystic formation in Figure 15 follows the lateral aspect of the tooth root, thus differentiating it from an apical cyst.
A cyst can continue to grow even after the irritation has ceased or the source has been removed. Such continuing growths are termed residual cysts.
Osteosclerosis and Condensing Osteitis
Increased bone deposition may be secondary to a variety of local irritants, most notable infection. Such increased bone deposits are termed osteosclerosis, or alternatively, condensing osteitis. Figure 16 illustrates the radiographic appearance of condensing osteitis surrounding the apices of a deeply carious first molar.
Although osteosclerosis is commonly associated with carious, frequently non-vital teeth, it may also be found at the apices of entirely normal teeth, most commonly the mandibular first permanent molar. It should be pointed out that involved teeth usually show fully formed roots without a significant degree of root resorption. (Other terms used to indicate condensing osteitis are rarefying or sclerosing osteitis.)
Osteoradionecrosis and Osteonecrosis
Osteoradionecrosis (ORN) also known as postradiation osteonecrosis (PRON) is a serious, debilitating and deforming potential complication of radiation therapy for the treatment of cancer. It is known to occur following radiation treatment when the maxilla or mandible is directly in the field of radiation.
Bisphosphonate-associated osteonecrosis of the jaw (ONJ) is uncommon but has been associated with intravenous bisphosphonate cancer therapy. Any necessary dental procedures should be completed before intravenous bisphosphonate cancer treatment is started. More research is needed for patients receiving oral bisphosphonate for the treatment of osteoporosis. At this time, it does not seem to be a serious risk and normal dental services are recommended.
Diagnosis depends primarily on clinical and radiographic changes in the bone. These signs and symptoms typically include ulceration of the mucosa, loosening of the teeth and exposure of necrotic bone.
Healing of Extraction Wounds
Normal Healing
Following normal tooth extraction, the extraction socket is clearly demarcated by the radiopaque bundle bone into which the periodontal ligaments had anchored the tooth. A radiographic image of a recent first mandibular molar extraction site is illustrated in Figure 17. Note the clear outline of the root socket.
With healing, new bone is deposited into the socket and, with time, the bundle bone slowly fades. After about 18 months, it can no longer be distinguished from the surrounding tissue.
Fibrous Healing
Occasionally dental extraction sites lay down a fibrous tissue healing. Such tissues appear as radiolucent areas such as that in Figure 18 and sometimes last for periods well in excess of the normal healing time.
Socket Sclerosis
If healing is accompanied by excessive bone deposition, socket sclerosis results, leading to radiodense areas within the socket as illustrated in Figure 19.
Residual Root Fragments
If the tooth is not completely removed, e.g., because of a root fracture or residual deciduous tooth root, a residual tooth fragment may persist. These fragments can be distinguished from socket sclerosis by the presence of a root canal and an intact periodontal ligament space. Figure 20 illustrates the appearance of a residual root and intact ligament space following the extraction of a mandibular first molar.
Fractures
Fractured Teeth
Traumatic injuries, extensive caries and oral neglect can lead to fracturing of the dental tissues. Maxillary incisors are particularly prone to traumatic injuries. The fracture often leads to losing portions of the tooth crown such as the traumatic loss of the incisal edges shown in Figure 21.
A crown fracture can also affect the tooth root, appearing as a radiolucent line across or with the tooth’s long axis. Be careful not to mistake the artifact of a fingernail crimp as a fracture! Figure 22 is a radiographic image of a fractured tooth. A fingernail crimp would be very similar, though possibly somewhat more broad and radiolucent (Figure 23).
Fractured Bones
Even though bone is usually strong and resilient, a forceful blow can cause it to break. Therefore, patients with a history of traumatic injury and a clinical picture of bruising and tenderness should be radiographed to detect a fracture. Depending on the nature of the injury, a fracture can be a straight or jagged line, which may penetrate partially or completely through the bone and leave the bones normally aligned or displaced. Figure 24 illustrates a non-displaced mandibular fracture in the canine region.
If the fracture site is unstable, or displaced, intraosseous wiring is used to maintain position during healing.
During healing, the body often lays down excess bone or callus in the injured area. This callus and retained intraosseous wiring is visible at the healed fracture site in Figure 25.
Developmental Abnormalities
Supernumerary Teeth
The relatively common abnormality of teeth numbering in excess of the standard 32 permanent or 20 deciduous is known as supernumerary dentition. Areas of the jaws most frequently affected with supernumeraries include the maxillary central and lateral incisor and molar regions, and the mandibular premolar region.
The most common supernumerary tooth is the mesiodens, occurring between the maxillary central incisors (Figure 26 and Figure 27). This tooth is usually small and cone-shaped and may be either erupted or impacted.
Supernumerary teeth of the maxillary molar region occur either distal to the third molar, thus called fourth molars, or between or adjacent to the third and second molars, becoming paramolars.
Multiple-impacted supernumerary teeth are classically associated with Gardner’s Syndrome, a hereditary condition marked by multiple polyps of the colon, and cleidocranial dysplasia, a rare hereditary condition in which there is defective ossification of the cranial bones and complete or partial absence of the clavicles. Given the serious ramifications of these diseases, it is vitally important to consider them whenever multiple supernumerary teeth are encountered.
Hypodontia (Too Few Teeth)
Missing teeth is an exceedingly common finding, which can usually be attributed to extraction or traumatic evulsion. Such acquired hypodontia must be contrasted with congenital hypodontia, which arises because of a developmental error.
Congenital hypodontia most commonly affects the third molars, the permanent maxillary lateral incisors and the maxillary and mandibular premolars. Frequently, hypodontia is bilateral. Figure 28 is an example of a patient with congenital hypodontia, affecting the mandibular second premolars bilaterally, the left mandibular first permanent molar, and retention and ankylosis of the mandibular second deciduous molars.
More severe forms of congenital hypodontia are associated with hereditary anhidrotic ectodermal dysplasia, a disease characterized by the absence of eyebrows and eye lashes; a depressed nasal bridge; prominent supraorbital ridges; light, scanty hair; and wrinkled palms, secondary to hyperkeratosis. In such patients, it is not uncommon for only three or four teeth to develop.
Macrodontia
Macrodontia is the formation of unusually large teeth. Most commonly, this developmental anomaly presents as a single enlarged tooth, and, less frequently, as multiple macrodonts. Figure 29 is a right maxillary lateral incisor macrodont with a small hypoelastic enamel defect on the labial tooth surface.
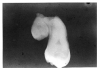
The patient’s radiographic image, shown in Figure 30 clearly outlines the macrodont and additionally reveals an impacted maxillary canine.
As noted earlier, macrodontia usually results in a single large tooth. Much less frequently, multiple macrodonts are encountered with such conditions as facial hemihypertrophy and pituitary giantism. Tooth fusion, which will be discussed later, produces teeth that are virtually identical to macrodonts; and, indeed, it may well be impossible to distinguish between the two.
Microdontia
Microdontia is a condition characterized by unusually small teeth. Again, it commonly affects only one tooth, most often the maxillary lateral incisor or peg lateral and the third molar. It may also manifest as a feature of other anomalies such as supernumerary teeth. Figure 31 is a maxillary third molar microdont.
Generalized microdontia is very uncommon. It has been associated with pituitary dwarfism, hypoplastic type amelogenesis imperfecta and anhidrotic ectodermal dysplasia.
Hutchinson’s Teeth
Hutchinson’s teeth result from a highly distinctive form of enamel hypoplasia, occurring only in congenital syphilis. Affected incisors demonstrate convergence of mesial-distal dimension approaching the incisal edge. Typically, there is a distinctive notch on the mid-incisal edge, which has been likened to the appearance of a screwdriver (Figure 32). All maxillary and mandibular incisors may show the defect, although the maxillary lateral incisor may appear normal while the others are defective.
Evagination
Evagination represents a somewhat rare dental developmental malformation in which there appears to be a small accessory cusp arising from the occlusal surface of a tooth. Figure 33 illustrates a maxillary premolar with evagination occupying the space between the buccal and lingual cusps.
Although it may occur on any tooth, it is most commonly observed on the premolars. The malformation is composed of enamel and dentin and may extend into the pulp; and thus, attrition on caries involving the evagination may lead to pulp necrosis and periapical disease.
Invagination (Dens in Dente)
Invagination represents a deep infolding of the tooth with extension of the enamel down through the dentin into the pulp. Such teeth can be severely deformed, appearing with an enlarged pulp chamber that has been likened to a tooth within a tooth (dens in dente).
The most commonly affected tooth is the permanent maxillary lateral incisor (Figure 34 and Figure 35). Single dens in dente are most common, but double varieties also occur.
Taurodontism and Pyramidal Teeth
Taurodontism is a fairly common developmental defect in which the affected multi-rooted teeth display apically displaced furcation, producing a pattern of large pulp chambers and short roots. Clinically, the teeth appear normal, but on a radiographic image, they demonstrate a distinct rectangular outline, such as seen in tooth #19 in Figure 36.
Taurodontism may affect multiple teeth, but it is limited almost entirely to the molars. It is associated with Kleinfelter’s Syndrome, a syndrome of gonadal defects, appearing in males with an extra X chromosome, which should be suspected whenever taurodontism is encountered in patients with unexplained mental retardation, a tall, thin appearance, long legs and arms, and a distinctly prognathic jaw.
Pyramidal teeth are morphologically similar to taurodontism. They exhibit enlarged, elongated pulp chambers but only single roots, as illustrated in tooth #18 in Figure 36. In effect, the condition appears to represent extreme apical displacement of the furcation, resulting in a single broad root, which, in actuality, is the body of the tooth. The clinician will sometimes encounter both taurodontism and pyramidal teeth in the same patient.
Dilaceration
Dilaceration is an unusual bend in the tooth root(s). The curvature usually results from trauma and can occur anywhere along the root. Since the tooth crown is clinically normal, the degree of dilacerations can only be detected radiographically.
Dilaceration may range from mild curvature, as in Figure 37 to severe bending, as in Figure 38.
The curvature is more visible if it occurs in a plane perpendicular to the central X-ray beam. If it occurs parallel to the beam, it casts a shadow similar to a radiopaque cyst or bone deposit because the axis is oriented toward or away from the beam.
Supernumerary Roots
Teeth having a greater number of roots than is anatomically typical have supernumerary roots. The canines, mandibular premolars and maxillary second premolars are usually single rooted, and a radiographic appearance such as that in Figure 39 would be diagnostic of supernumerary roots.
Fusion and Gemination
Fusion is defined as the joining of two originally separate teeth through the dentin, or through the dentin and enamel. In contrast, gemination represents incomplete division of what should have been two separate teeth. Fusion may involve supernumerary teeth, and gemination may occur in quadrants also affected by partial anodontia; thus, counting the teeth in the affected area is of limited diagnostic value. Regardless of which process initiated the error, it is practically impossible to distinguish between fusion and germination, and in either case, the tooth will appear much like that in Figure 40.
The distinction between fusion and germination is primarily of academic interest and thus, the etiology is of less clinical concern than is the presence of the condition and the potential ramifications involved.
Concrescence
Concrescence represents the joining of adjacent teeth via the cementum with obliteration of the intervening periodontal ligaments. Concrescence is usually found in two teeth, rarely in three or more. The clinical appearance of the condition is shown in Figure 41 and the appearance on a radiographic image in Figure 42.
Regional Odontodysplasia
Regional odontodysplasia represents a developmental disorder in which one or several teeth in a contiguous group fail to properly form. The condition occurs sporadically without a distinct familial pattern and most commonly affects the anterior maxillary quadrants. The involved teeth often fail to erupt, or if they do erupt, they are misshapen with irregular crowns and defective mineralization. Unerupted teeth are characterized by soft tissue swelling and painful symptoms.
Radiographic features typically consist of one tooth, or segment of teeth, demonstrating incomplete formation and reduced radiopacity. Because of their radiolucency, they are sometimes known as ghost teeth. In Figure 43, the posterior mandibular segment demonstrates an unerupted and incompletely mineralized second premolar and second molar. The first molar is absent and swelling of the overlying soft tissue is noted.
Dentinogenesis Imperfecta and Dentin Dysplasia
Dentinogenesis Imperfecta is an inherited disorder, usually showing a dominant autosomal pattern. Clinically, the teeth have a peculiar translucent appearance with discoloration ranging from brown to yellow to gray. Such teeth are termed opalescent.
Radiographically, all teeth in the deciduous and permanent dentitions show early and frequently complete obliteration of the pulp chambers and canals with short, blunted roots (Figure 44).
Dentin dysplasia is another autosomal dominant condition in which there is markedly disturbed dentin formation. This extremely rare condition occurs in two distinct patterns. The first, referred to as radicular dentin dysplasia, is characterized by partial or complete obliteration of the pulp chamber and extremely short, blunted roots (Figure 45). When persistent, the pulp chamber displays a characteristic crescent.
The second type is coronal dentin dysplasia and is characterized by the thistle-funnel pulp chamber enlargement in the permanent teeth (Figure 46).
Amelogenesis Imperfecta
Amelogenesis Imperfecta constitutes a diverse group of distinct, genetic disorders which share generalized defective enamel formation. As distinct conditions, varieties of amelogenesis imperfecta have been linked to autosomal, X-linked, dominant, and recessive genes.
Clinically, the enamel may be partially missing (hypoelastic); very soft (hypocalcified); or firm but chippable (hypomaturation). Varying degrees of yellow to brown tooth discoloration may be present. On the radiographic image, the teeth may show hypoplasia from failure of enamel formation or a chipped and worn-away appearance from partial formation, as in Figure 47.
In cases of hypocalcification, the radiodensity of the enamel and the dentin are very close and, thus, delineating between them is difficult.
Turner’s Tooth and Environmental Hypoplasia
Enamel hypoplasia, limited to a single tooth, is known as Turner’s Hypoplasia and the affected tooth is termed Turner’s tooth. The most frequently affected teeth are the permanent maxillary incisors and the maxillary and mandibular premolars. Common causes for the condition include local trauma or infection derived from an overlying deciduous tooth. Clinical appearance can range from mild, opaque chalkiness or brown discoloration or frank enamel pitting such as that in Figure 48.
In contrast to the genetic nature of Turner’s Hypoplasia, environmentally-induced developmental failure of enamel formation affecting multiple teeth is termed generalized environmental enamel hypoplasia. Environmental factors can include nutritional deficiencies, excessive fluoride ingestion, and severe, fever-producing childhood diseases.
Clinically, the affected teeth show localized enamel deficiency ranging from focal opacification to severe pitting. The distribution of enamel defects reflects the chronology of enamel formation with most severely affected areas representing the area that were forming at the time of the environmental influence.
The radiographic features of generalized environmental enamel hypoplasia consist of linear bands of relatively radiolucent enamel, as in Figure 49. Mild opacification and focal surface pitting may not be visible on radiographic images.
Talon Cusp and Enamel Pearl
The talon cusp represents a developmental anomaly in which a peculiar lingual cusp forms on the maxillary or mandibular incisors. When small, the cusp cannot be distinguished from an accentuated cingulum. When well-developed, the cusp appears clinically, as illustrated in Figure 50 and, on a radiographic image, as in Figure 51.
The enamel pearl is a misplaced (ectopic) globule of enamel, occurring most commonly in the furcation areas or near the cementoenamel root surfaces of the molar teeth. Affecting the maxillary more often than the mandibular areas, the relatively rare enamel pearls may contain a dentin core, occasionally with pulpal extension.
Radiographically, the pearl appears as a round or semi-spherical area of increased radiodensity. When occurring on the mesial or distal aspects, the pearl produces an obvious convex profile. On the buccal or palatal/lingual aspects, it is less easily seen and may resemble pulp stones.
Regressive Changes in Teeth
Attrition
Attrition represents the physiologic wearing away of tooth structure through such causes as normal mastication. The incisal, occlusal and interproximal surfaces are typically affected, and often the enamel is worn away so that the exposed dentin is clearly visible. Although attrition rarely results in serious disease, advance cases can lead to pulp necrosis and periapical disease.
Abrasion
The pathologic wearing away of tooth structure secondary to friction is abrasion. Agents, which contribute to abrasion include abrasive toothpaste; improper use of a toothbrush, flosses, and toothpicks; and personal habits such as excessive brushing, and holding pins, nails, and tacks between the teeth. A common form of abrasion involves the cervical areas, producing a sharply defined V-shaped defect such as that crossing the buccal aspect of the premolar in Figure 52.
Erosion
Erosion represents loss of tooth structure caused by chemical action. Usually these chemicals are acidic and the process does not involve bacterial action. Clinically, erosion is usually described in connection with the gingival one-third of the labial aspect of the anterior teeth, although any tooth surface can be affected. Erosion may arise due to environmental factors such as personal diet and occupations that involve working with acids.
Chronic vomiting may produce extensive erosion of the lingual tooth surfaces due to the acid nature of stomach contents. This type of erosion is illustrated in Figure 53.
Pulp Stones
Pulpal calcification is an extremely common finding and is considered by many to be a variation of normal pulpal development. Calcifications presenting as distinct intra-chamber (or less often intra-canal) radiopacities are known as pulp stones. Figure 54 illustrates a prominent stone in the pulp chamber of the second maxillary molar. It must be noted that it is often difficult to differentiate the radiographic appearance of a pulp stone from the simple superimposition of furcation contours.
Hypercementosis
Excessive deposition of cementum along the root surface is termed hypercementosis. The precise cause of this condition is not well understood, although the loss of tooth antagonism and local inflammation is often associated with it. A special exception is osteitis deformans or Padget’s disease, in which teeth in an affected jaw typically demonstrate a remarkable degree of hypercementosis.
Radiographically, the condition is characterized by a bulbous, opaque expansion of root contours, usually in volving much of the root length while preserving the periodontal ligament space and lamina dura as in Figure 55. Less commonly, the overgrowth is limited to the root apex.
Ankylosis
Tooth ankylosis represents a direct union of tooth to bone, eliminating the normally interposed periodontal ligament. Ankylosis is uncommon, usually encountered with deciduous teeth and often, though not exclusively, associated with local trauma and/or infection.
Clinically, deciduous ankylosis typically presents a retained tooth positioned below the level of the occlusal plane and is termed a submerged tooth. Radiographically, the ankylosed tooth typically exhibits signs of partial root resorption, obliteration of portions of the periodontal ligament, mild osseous sclerosis and apparent direct attachment of root and bone (Figure 56). On occasion, impacted teeth will become ankylosed in the jaw.
External Resorption
Mild external resorption of permanent teeth is a relatively common finding. Its specific causes can often be attributed to trauma, orthodontic therapy, reimplantation, cysts, tumors and infection. In other cases, no specific cause can be identified.
Root resorption most commonly is limited to the apical portion of the root and lacks any clinical manifestations. However, the condition can advance to the point that teeth become mobile and exfoliate.
Radiographic appearances include blunting of root apices with shortening of root length. In some cases, abrupt loss may be noted, and with advancing disease, the entire root may appear lost. Figure 57 illustrates a marked blunting and root loss following orthodontic therapy.
It is critically important to examine the tissues immediately surrounding the resorbing root. While, in most cases, the resorption is mild and relatively inconsequential, it can be severe and may be secondary to a number of significant tumors, including odontogenic neoplasms and metastatic cancer. Care must be taken to avoid simply identifying the condition without making a thorough investigation for signs of a far more serious disease.
Internal Root Resorption
Internal resorption represents a peculiar internal dissolution of dentin, which can extend eventually into the enamel and/or cementum by the tooth root. Usually, only a single tooth is involved, and although the cause is not clearly understood, it is often linked to inflammation.
Clinically, internal resorption in the pulp chamber may lead to the Tooth of Mummery with a developing pink hue in the tooth crown. Resorption in the root canal is not clinically visible; however, perforation of the root usually requires that the tooth be extracted.
Radiographic evidence of internal resorption consists of an unusual widening of the pulp chamber or canal as shown in Figure 58. If the canal is involved, it is virtually impossible to distinguish between internal and external resorption.
Developmental Anomalies of the Jaws
Mandibular Tori
Mandibular tori represent benign overgrowths of mature, lamellar bone, occurring on the lingual mandibular cortex. Typically attached to the mandible opposite the premolar region and superior to the mylohyoid line, they are most commonly bilateral. There is some variation in incidence among races with a higher incidence among Orientals than in Caucasians. Apparently, genetic factors also influence tori development, as the offspring of parents with mandibular tori have a much higher incidence of development.
Radiographically, tori appear as well-defined areas of radiopacity overlying the tooth roots (Figure 59), particularly extending from the canine to the molar regions. If tori are seen on radiographic images, they should be clinically confirmed in order to rule out other conditions, which lead to osseous radiopacity.
Maxillary Torus
The maxillary torus presents as a hard, frequently lobulated, benign overgrowth of mature lamellar bone. It is frequently located in the midline of the hard palate (Figure 60) and attached by a broad, bony base.
The condition is more common in Native Americans, American Indians and Eskimos than in Caucasians or Blacks and has a population-wide frequency of occurrence of about 25 percent. Hereditary factors have been implicated. Radiographically, the maxillary torus appears as a well-defined radiopacity situated at, or superior to, the apices of the maxillary teeth as in Figure 61. On panoramic radiographic images, it may be visualized in the midline and over the roots of the canines, premolars and molars.
Stafne Bone Cavity
The Stafne cavity is an osseous defect caused by pressure of the submandibular salivary gland on the mandible during its development. It is a well-defined radiolucency found at the angle of the mandible below the mandibular canal that has no significance except in its differentiation from other conditions (see Figure 62).
Clefts
Developmental clefts of the palate are not uncommon. They result from a smooth defect and are often associated with marked tooth displacement.
Summary
Many conditions of the hard and soft tissues of the oral cavity and surrounding area can be diagnosed and treated through the use of quality, diagnostic dental radiographic images. The importance of quality dental radiographic images cannot be overstated and is covered in other continuing education courses offered by the American Dental Assistants Association. It is important that the whole dental team have the ability to recognize anomalies shown in radiographic images. Early detection of any dental disease offers the best prognosis for the patient and continues the quality of care every patient deserves.
GLOSSARY
abrasion – pathological wearing away of the surface layers of hard or soft tissues
anomaly – abnormality
apical foramen – an opening at a tooth’s root tip that allows the entry of nerve and blood vessels to the pulp
attrition – wearing away by friction or rubbing
autosoma – pertaining to a chromosome other than a sex chromosome
bilateral – two sided
cementoenamel junction – the meeting of the enamel of the crown and the cementum of the root at the cervix of a tooth
chronic – persisting over a long period of time
dysplasia – abnormal growth or development of cells, tissue, bone, or an organ
ectopic – out of place; e.g., an ectopic tooth eruption is one that occurs outside the normal path
embrasure – the V-shaped space between curved adjacent surfaces of teeth
epithelial – type of tissue that forms the covering of all body surfaces
erosion – the destruction of tooth substance by chemical or mechanical-chemical action
exfoliate – to shed teeth, particularly referring to primary teeth
exudate – a liquid substance that oozes from blood and lymph vessels, typically as a result of inflammation
fibrous – composed of or containing fibers
furcation – the point at which the roots of multi-rooted teeth separate
gonadal – pertaining to the ovaries or testes
granuloma – a tumor that is filled with granulation tissue
hemihypertrophy – an excessive growth of one half of the body, an organ, or a part (e.g., facial hemihypertrophy)
incipient – the beginning stage; e.g., incipient caries is the beginning stage of tooth decay when the decay has not yet completely penetrated the enamel
intraosseous – within bone
lamina dura – the compact bone that lines the tooth sockets
lobulated – divided into lobes, subdivisions
necrosis – the death of cells or tissues
opalescent – a translucent appearance
orifice – the entrance or outlet of any body cavity
osseous – bony or of bone-like structure or consistency
ossification – the formation of bone or a change into bone
pathosis – a disease condition
periodontium – a collective term that denotes the tissues surrounding and supporting the teeth; includes 1) the gingiva, 2) the cementum of the tooth root, 3) the periodontal ligament, and 4) the alveolar bone
polyp – a general term that describes any mass of tissue that bulges or projects outward or upward from the normal surface level
prognathic – pertaining to a forward relationship of the jaws to the head (anterior to the skull) resulting in a protruding lower face
radiodensity – the degree of radiolucency or radiopacity of a substance or tissue
radiolucent – a term that describes the ability of a substance or tissue to allow passage of radiation with relatively little attenuation (reduction of energy) resulting in a darker image on a finished radiographic image
radiopaque – a term that describes the ability of a substance or tissue to attenuate (reduce or slow) the energy of radiation that passes through it resulting in a lighter image on a radiographic image
sclerosis – hardening of a body tissue
scurvy – a condition that results from an ascorbic acid (vitamin C) deficiency; common symptoms include weakness, poor wound healing, and hemorrhage under the skin and mucous membranes
suppurative – forming pus
taurodontism – an anatomical abnormality in which a tooth’s pulp chamber is elongated, enlarged, and extends into the region of the roots
REFERENCES
Bath-Balogh, M. and Fehrenbach, M. (2011) Illustrated Dental Embryology, Histology, and Anatomy. (3rd ed.) Elsevier Saunders.
Bird, DL. and Robinson, DS. (2012) Modern Dental Assisting. (10th ed.) St. Louis, MO: Elsevier Saunders.
Iannucci, J. and Jansen-Howerton, L. (2012). Dental Radiography Principles and Techniques. (4th ed.) St. Louis, MO: Elsevier Saunders.
Scheid, R. and Weiss, G. (2012). Woelfel’s Dental Anatomy: Its Relevance to Dentistry. (8th ed.) Baltimore, MD: Lippincott Williams & Wilkins.
ABOUT THE AUTHORS
Allan G. Farman, BSD, EdS, MBA, PhD
Allan G. Farman is a Diplomate of the Board of Oral and Maxillofacial Radiology, and Professor of Oral and Maxillofacial Radiology in the Department of Primary Patient Care at the University of Louisville School of Dentistry.
Revised 2017
Members of the Council on Education of the American Dental Assistants Association helped with the revision of this course. All members of the Council on Education are ADAA Active or Life Members with an interest in dental assisting education. Each one volunteers their time to the lifelong learning of dental assistants.