You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
The ADAA has an obligation to disseminate knowledge in the field of dentistry. Sponsorship of a continuing education program by the ADAA does not necessarily imply endorsement of a particular philosophy, product, or technique.
Approximately 49,750 people in the US will be newly diagnosed with oral cancer in 2017. For more than a decade there has been an increase in the rate of occurrence of oral and oropharyngeal cancers. Though thought by some as a rare occurrence, every single day in the United States alone, 132 new individuals are diagnosed and one person dies from oral cancer every hour of every day. Rates of past occurrence do not have to predict the future.1
The wonderful part of predictions are that they can be wrong. The dental healthcare team can make plans to circumvent that future death rate, not by being reactive, rather by more proactively identifying risks for oral precancer.
Adaptable Brains
Our adaptable brains allow us to make profound positive changes; altering language is the first real action step toward change. There are many excellent publications available on the diagnosis and management of oral cancer. A new textbook, Oral Precancer, edited by Peter Thomson (Wiley-Blackwell 2012) concentrates on the recognition of oral precancer as its title indicates. Yet, identification of oral precancer is much more than a simple change of language. It is a profound change in "diagnosis and management of the discrete, readily identifiable oral mucosal lesions and the more widespread systemic conditions that may affect the lining of the oral cavity and whose clinical presence may precede the development of invasive oral cancer."2
What Is Precancer?
Identifying oral precancer is a spectrum from ascertaining patient risk factors to identifying the most inconspicuous change in tissue color, consistency, or contour. The dental healthcare team members that are focused on prevention and precancer detection are progressively taking action to ensure that their patients have been educated and advised. They are having discussions with their patients that lead to identifications of risk factors. Identifying precancer is more than palpating the submandibular nodes and more than satisfying the oral cancer screening according to seemingly thorough protocols. These dental healthcare team members have challenged themselves to bring an oral precancer protocol (not just a screening) to the next level of comprehensiveness and take their responsibility of oral precancer detection very seriously.
Early Intervention
Early intervention has been defined as "services given to very young children with special needs, generally from birth until the child turns three years of age. Services include speech therapy, occupational therapy and physical therapy, provided either in an office or in the child's home. The hope is that these services, provided early, will address any delays in development so that the child will not need services later on."3 Patients are not limited to children; early intervention should be ongoing throughout patients' lifespan.
An early interventionist should have the qualities of patience, perseverance, empathy, flexibility, consistency, and a love of teaching. Necessary skills include organization, self-management, and communication.4 Those qualities describe the function and skill set of a dental healthcare team member. The dental healthcare team can intervene to guide a child into a caries-free future, or guide an adult into lifelong periodontal health. Borrowing the interventionist term from the medical field, the dental professional should borrow another one: the well-baby visit. Let's expand the term to the well-person visit. Each dental professional should stop the old paradigm that dentistry is about repairing tissue affected with disease. With the dental tools we have in the examination arsenal these days, dentistry can - and should - be about dental wellness. Any time an early anomaly is detected, it can make a huge difference in the outcome.
The unfortunate reality is that dentistry is stuck in the paradigm, "if it ain't broke, don't fix it." As with any belief, boundaries block our view. The word prevention is overused and has lost its true meaning. Lack of quantifiable symptoms has meant traditionally equalled health. That is a circular argument: define health: lack of disease. Health is a continuum (Figure 1). The majority of currently used detection modalities are looking for moderate to advanced disease shown on the far right side of the continuum identified as "tertiary." That is where dentistry is currently halted. Early interventionists work in all parts of the continuum leading to updated definitions of prevention.
Early Interventionist definitions of prevention:2
- Eliminating the principal risk factors
Does WNL Truly Mean "Within Normal Limits?"
Abbreviations can a useful communication tool when there is a key to the meanings of those abbreviations. The dental healthcare team can easily fall into believing that the abbreviations used daily are universal. They are not. Abbreviations can mean different things to different people. One common abbreviation is WNL. Most often, WNL stands for within normal limits but does it mean that? Unfortunately, all too often it stands for "we never looked." This seems to particularly be the case with oral cancer screening. It is the belief of this author, when full documentation of all conditions present is combined with risk assessment; the majority of the time, WNL is used inaccurately.
In the year 2000, an American Dental Association survey reported that a majority of dental practitioners claim to conduct regular oral cancer screenings; yet only 15% of patients report receiving an oral cancer examination.5 Late in 2007, the Crown Council along with OraPharma, 1-800 Dentist, and Oral Health America commissioned and funded a scientific, national public opinion survey meant to identify the public's perceptions of dental health and the role dentists play in providing dental health services.6 The results showed 85% of the survey respondents indicated that it was important to them that their team of dental professionals check for oral cancer. Yet, only 51% of the survey respondents indicated that their dental professionals actually did so. That means that 1/3 of those surveyed were expecting something that they were not receiving.
It is hard to estimate how much the general population knows about oral cancer. Interest concerning this type of cancer has increased. Michael Douglas helped gain visibility with the public with his open discussion about his battle with cancer, sharing several personal and intimate details about how it developed and how his treatment was progressing. In 2013, the actor admitted he lied saying he had throat cancer on the urging of his physician. He had human papilloma virus-related tongue cancer, but lied about it because of fears that the potential treatment could be disfiguring, resulting in harm to his career.29
HPV Connection
In the past three decades, a 60% increase in oropharyngeal cancer has been detected in people under age 40. This information, along with the 25% of oral cancer cases with no known risk factors, caused researchers to look for new possible causes.7-8 Human papillomavirus (HPV) has been known to cause cervical cancer. But, until now, its connection with oral cancer was based primarily on molecular data. An epidemiologic study published in May of 2007 in the New England Journal of Medicine, and many other subsequent publications, have provided compelling support for this relationship. The statistics on HPV are staggering with approximately twenty million people currently infected with HPV. The most dangerous type of HPV, known as HPV 16, is transmitted through sexual contact.9-11
An April 2011 PR Newswire headline quoting the Oral Cancer Foundation (www.oralcancerfoundation.org) alerted the public: "HPV Now the Leading Cause of Oral Cancers in the US."12 Even conservative predictions estimate that 70% of oropharyngeal cancers in 2020 will be HPV positive.13
HPV is the most commonly transmitted sexual disease with an increase between 1988 and 2004 of 225%.14 Even with those realities, 70% of Americans know nothing about HPV as a sexually transmitted disease (STD) and:
• Condoms do not protect from HPV,
• HPV does not appear on standard STD tests, and
• There is no pharmacologic cure for HPV.14
Over half of all adults will have had this infection over their lifetimes. The good news for most people is that they clear the HPV infection and develop natural immunity to the HPV type that caused their infection. It takes years for an HPV-related cancer to develop after infection with the virus.15 At the same time, the detection of HPV may ultimately serve a more comprehensive role than as a risk factor. HPV may be the most important link in determining all aspects of a patient's care from early detection to more accurate disease staging and care planning.
Patients typically present with a sore throat, ear pain, painful swallowing, or hoarseness, and on physical exam they often have lymph node involvement in the neck. The highest risk sites are at the base of the tongue and the tonsillar area. Palpation of the neck has never been more important. The highest frequency of HPV-positive cancer is related to oral sex and to the number of partners. Figure 2 shows an example of cancer, found on the buccal mucosa.
Is Age a Risk Factor?
Age has often been listed as the major risk factor in oral cancer. Upon closer investigation, this belief does not hold up. Cancers are ranked into stages depending on the extent of their growth and spread through the body; stages correspond with severity. Determining the stage of a given cancer helps physicians to make treatment recommendations. Cancers are commonly ranked into five progressive stages: 0, I, II, III, and IV. Stage 0 cancer is cancer that is just beginning, involving just a few cells. Stages I, II, III, and IV represent cancer as it progressively advances.16 Late diagnosis placed in stages III & IV accounts for 70% of all diagnoses. As stated on the Oral Cancer Foundation website, "Historically the death rate associated with this cancer is particularly high not because it is hard to discover or diagnose, but due to the cancer being routinely discovered late in its development." It is not age that is the risk factor, it is the late diagnosis.
HPV infections are different and age seems to make a difference. A younger person has a higher chance of getting an HPV infection but also a higher chance of clearing it. After the age of 30, infection risk becomes lower, that is the good news. The bad news is the chances of clearing the infection are also lower. When a person gets an HPV infection when older, there is a higher likelihood for it to be persistent and progress to a more serious condition.17
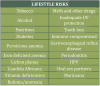
Table 1 shows a list of other lifestyle risk factors for oral cancer. Some bear a more detailed explanation.
Tobacco and Alcohol
The harm of tobacco use is well-known, including to those still engaging in the use. There are several types of tobacco consumption: cigarettes, chewing tobacco, pipes and cigars, snuff, and hookahs. The U.S. culture has made tobacco use such a taboo to the extent that it may prevent users from asking for help to quit the habit. It can be easy to fall into judgment and make condescending and rude comments. This type of communication does little to help a tobacco user who needs to stop.
Most professionals are aware that heavy restrictions were imposed as part of the national litigation settlement on tobacco companies. There are numerous programs to assist tobacco users such as Quit For Life® from the American Cancer Society (www.quitnow.net). There is a dental insurance code in the 2013 Current Dental Terminology (CDT) book - code D1320 - which the dental team can use for insurance help when employing tobacco counseling for the control and prevention of oral disease.18 Under some policies, these services can be paid. Whether or not it is covered by insurance, this should not have any bearing on dental professionals offering tobacco cessation information.
Alcohol abuse is a major risk factor associated with the development of oral cancer. Alcohol's effect on the mouth may be the key to understanding how it combines with tobacco to increase the risk of developing cancer. The dehydrating effect of alcohol on the cell walls enhances the ability of tobacco carcinogens to permeate mouth tissues. Additionally, nutritional deficiencies associated with heavy drinking can lower the body's natural ability to use antioxidants to prevent the formation of cancers.
Tobacco and alcohol are essentially chemical factors, but they can also be considered lifestyle factors, since people also have some control over them. Besides these, there are physical risk factors such as exposure to ultraviolet radiation. This is a causative agent in cancers of the lip, as well as other skin cancers.
Further research is necessary to determine the relationship between oral cancer, alcohol and tobacco use. It is widely accepted that eliminating the use of tobacco, and reducing or eliminating the intake of alcohol, will immediately reduce the risk of developing oral cancer. For 10 years, the risk still remains higher than for a non-drinker/never-smoker.19 This time window must be considered when evaluating risk factors.
One further note, most health histories have a question regarding alcohol use. Further questioning may be appropriate. Binge drinking18 in younger women is increasing. Chronic use of alcohol is defined as:
• 3 oz. spirits/day
• 2 beers/day
• 1 glass of wine/day
Nutrition
There are studies which indicate a diet low in fruits and vegetables could be a risk factor, and that conversely, one high in these foods may have a protective value against many types of cancer. Certain food components seem to help prevent cancer and sometimes even assist the body in fighting the disease. Researchers call these chemo-protective agents, including a group commonly known as antioxidants. They appear to protect the body from the effects of carcinogenic elements. One thing is for certain, it is never wrong to eat plenty of fresh fruits, vegetables, and whole grains. These are the primary sources of the nutritious elements the body needs to maintain a healthy and competent immune system, the primary defense against cancer and other illnesses.
Periodontitis Linked to Head and Neck Oral Cancer
In May of 2007, researchers from State University of New York (SUNY) at Buffalo and the Roswell Park Cancer Institute showed for the first time that an association exists between history of periodontitis and the risk of tongue cancer.20 The link between chronic inflammation and cancer has been suspected for many years. Mine Tezal, D.D.S., Ph.D., assistant professor at SUNY and the first author of this study said,
"Chronic inflammation has been associated with cell proliferation, cell survival, cell migration and angiogenesis, all of which promote tumor development. To determine these roles more specifically in oral cancers, future studies with more participants and more sensitive clinical diagnoses are needed to generate more complete answers."21
This research brings into sharper focus the need for appropriate, early diagnosis and treatment of periodontal disease in addition to the recognition of periodontal disease as an added risk factor for oral cancer.
In 2012, Dr. Tezel et al, published a follow-up study stating,
"The results of this study provide the first evidence, to our knowledge, of an association between chronic periodontitis and HNSCC based on an objective and quantitative measure of periodontitis history. The strength of the association was greatest in the oral cavity, followed by oropharynx and larynx. The association persisted in patients who never used tobacco and alcohol but it was strongest in former smokers. Furthermore, this study suggests that periodontitis history is associated with poorly differentiated tumors in the oral cavity."22
This means, all members of the dental healthcare team need to take a new look at the risk factors considered for oral cancer which now includes periodontal disease.
Cannabis
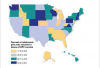
The vast majority of HPV-positive cancers lack association with the traditional risk factors, tobacco and alcohol. The risk of HPV-positive head and neck tumors has been associated with sexual behavior including increasing numbers of both vaginal and oral sex partners, young age at first intercourse, and history of genital warts. Several studies found that the risk of developing an HPV-16 positive head and neck cancer increased with increased marijuana use.23 The changing behaviors in both tobacco use and sexual practices in the U.S. is well-known. What is also well-known are the number of states allowing and/or considering legal use of cannabis. (Figure 5)
HPV Vaccine Controversies
The Centers for Disease Control and Prevention (CDC) has recommended the HPV vaccination series for preteen girls since 2007.25 Only about 1/3 of eligible girls in the United States have received the vaccine, with many of those not finishing the 3-injection series over the 6 months time frame.26 Studies in 2013 are showing HPV vaccine rates are in decline. Some have suggested reducing the age to give the vaccine to a time prior to the child's awareness of the sexual implications.
The HPV vaccine has been controversial since its introduction. Interested parties in the discussion include: Businesses (drug companies), Professionals (health care), Religious (pastors, rabbis & priests), Political (politicians & community leaders) and the Parents and their children. Whatever the point of view, each believe they are acting in best interests. Discussions are particularly difficult when human sexuality, implications of science, and ethical beliefs collide.17 Humans base opinions on past experiences, religious beliefs, biases, preconceived ideas and culture of a society.
Prior to the dental healthcare team making recommendations on the vaccine, reading the 2008 book, The HPV Controversy: Sex, Cancer, God, and Politics,17 may be helpful in understanding the controversies. Being open-minded and accepting during discussions to others that think differently provides opportunities for education versus attempting to shove individual opinions on others which most often does not lead to change.
Becoming Risk Factor Managers
The risk factors discussed in this article are the modifiable lifestyle factors. There are other non-modifiable factors for oropharyngeal cancer. Risk assessment takes all known risk factors into account. Using a systematized method can assist dental professionals in determining overall risk. A variety of systems are available.
Dental insurance carriers understand risk assessment. In April 2013, Delta Dental, the nation's largest dental benefits company, took another step helping people assess their risk for oral diseases. "Risk assessment is an important first step for people who want to educate themselves on the state of their oral health," said Dr. Bill Kohn, vice president of dental science and policy for Delta Dental. Delta Dental now offers PreVisers Corporation's mydentalscore.com to its 60 million subscribers.27
Summary
All dental care professionals need to educate themselves and their patients about the relationship between oropharyngeal cancers, HPV, and risk factor management. A Risk Factor Manager28 is an early interventionist whose tasks are performing diagnostic testing, gathering data, and putting it into a meaningful report for the care providers. Risk Factor Managers practice on all three levels of prevention including proactively identifying risks for oral precancer with the hope of changing our dread predictions.
Glossary
antioxidant - a substance, such as vitamin C or E, that removes potentially damaging oxidizing agents in a living organism
carcinogenic - cancer-causing
HNSCC - head and neck squamous cell carcinoma
hookah - a tobacco pipe of Near Eastern origin with a long, flexible tube by which the smoke is drawn through a jar of water and thus cooled
HPV - human papilloma virus
malignant - tending to invade normal tissue or to recur after removal; cancerous
morbidity - rate of incidences of a disease
mortality - death rate, especially of large numbers; heavy loss of life
oropharyngeal cancers - cancer that forms in tissues of the oropharynx (the part of the throat at the back of the mouth, including the soft palate, the base of the tongue, and the tonsils)
palpation - physical examination in medical diagnosis by pressure of the hand or fingers
paradigm - a typical example or pattern of something; a model
precancer - from identifying patient risk factors to identifying the most inconspicuous change in tissue color, consistency or contour
risk factor - a condition that increases a person's chance of getting an illness or disease
About the Author
Patti DiGangi, RDH, BS
Patti DiGangi, RDH, BS graduated from William Rainey Harper Dental Hygiene and received her Bachelor of Science degree in Health Care Leadership from National Louis University. She continues to take an active future-oriented leadership role in a variety of professional organizations. She is the Dental Corporate Chair for the Oral Cancer Foundation Walk for Awareness of Northern Illinois and has been speaking and writing on the early detection and prevention of oral cancer for many years.
Patti believes dentistry is no longer just about fixing teeth; dentistry is indeed oral medicine. Her diligent work helps dental professionals embrace the opportunities and understand the metrics that accurate insurance coding provides. In fact, the American Dental Association recognized her expertise by inviting her to write a chapter in its CDT 2017 and 2018 Companion books. Patti holds publishing and speaking licenses with the ADA for Current Dental Terminology, 2017 as well as SNODENT, 2017 diagnostic coding. She is the author of DentalCodeology, which is a series of easy-to-read, bite-sized books.
References
1. Oral Cancer Foundation website. Available at: http://oralcancerfoundation.org/. Accessed 5/9/17.
2. Thomason, P. Oral Precancer: Diagnosis and Management of Potentially Malignant Disorders. (2012) Hoboken, NJ: Wiley-Blackwell.
3. Special children: About.com. Available at: http://specialchildren.about.com/od/earlyintervention/g/El.htm. Accessed 4/29/13.
4. Southeastern Louisiana University Master of Arts program in teaching program, Early Interventionist. Available at: http://selu.edu. Accessed 4/29/13.
5. Horowitz AM, Drury TF, Goodman HS, et al. Oral pharyngeal cancer prevention and early detection. Dentists' opinions and practices. J Am Dent Assoc. 2000;131:453-462. http://www.oralcancerfoundation.org/dental/pdf/dentist_opinions.pdf Accessed 4/10/13.
6. Anderson, S. What Patients Really Want: The Public Opinion Survey on Dentistry and what you need to do now. Total Patient Services Institute. 2007. http://www.crowncouncil2.com/downloads/What%20Patients%20Really%20Want%20SR.pdf Accessed 4/1/13.
7. Rates of occurrence in the United States. February 2006. The Oral Cancer Foundation Web site. Available at: http://www.oralcancerfoundation.org/facts/. Accessed 4/29/13.
8. Head and neck cancer. November 2005. Oncology Channel Web site. Available at: http://www.oncologychannel.com/headneck/index.shtml. Accessed 4/29/13.
9. D'Souza G, Kreimer AR, Viscidi R, Pawlita M, Fakhry C, Koch WM, Westra WH, Gillison ML. "Case-control study of human papillomavirus and oropharyngeal cancer" N Engl J Med. 2007 May 10;356(19):1944-56. Available at: http://eglobalmed.com/opt/AmedeoLiteratureGuide/content.nejm.org/cgi/reprint/356/19/1944.pdf. Accessed 4/29/13.
10. Human Papillomaviruses and Cancer: Questions and Answers. June 8, 2006. National Cancer Institute. Available at: http://www.cancer.gov/cancertopics/factsheet/Risk/HPV Accessed 4/29/13.
11. Fakhry, C., Gillison, M. Clinical Implications of Human Papillomavirus in Head and Neck Cancers J Clin Oncol 2006 24: 2606-2611 Available at: http://www.oralcancerfoundation.org/facts/pdf/clinical_implications_2006.pdf Accessed 4/29/13.
12. HPV Now the Leading Cause of Oral Cancers in the US. PR Newswire. April 4, 2011. http://www.prnewswire.com/news-releases/hpv-now-the-leading-cause-of-oral-cancers-in-the-us-119168359.html. Accessed 4/29/31.
13. Wendling. P. HPV-Related Oral Cancer Incidence Spikes Sharply. The Oncology Report. June 4, 2011. http://www.oncologypractice.com/oncologyreport/specialty-focus/head-neck/single-article-page/hpv-related-oral-cancer-incidence-spikes-sharply.html Accessed 4/29/13.
14. Hariri S, Unger ER, Sternberg M, et al. Prevalence of genital human papillomavirus among females in the United States, the National Health and Nutrition Examination Survey, 2003-2006. J Infect Dis. 2011;204:566-573. http://168.105.175.200/Katz2012/Hariri%20HPV%20prevalence.pdf Accessed 4/29/13.
15. Prystowsky, M. Dr. Michael B. Prystowsky responds to The Annual Report to the Nation on the Status of Cancer 1975-2009. YouTube January 29, 2013. https://www.youtube.com/watch?v=Cz1Ha_XbhAY Accessed 4/29/13.
16. Cancer Staging. National Cancer Institute. http://www.cancer.gov/cancertopics/factsheet/detection/staging. Accessed 4/29/13.
17. Krishnan, S. The HPV Controversy: Sex, Cancer, God, and Politics. Praeger: Westport, CT. 2008.
18. DiGangi, P. Dentalcodeology: More than Pocket Change. Mini-Buks: Phoenix, AZ. 2013.
19. Oral Cancer Facts. Oral Cancer Foundation. http://www.oralcancerfoundation.org/facts/ Accessed 4/29/13.
20. Alcohol and Public Health. Centers for Disease Control. November 7, 2012. http://www.cdc.gov/alcohol/faqs.htm#bingeDrinking Accessed 4/29/13.
21. Tezal,M., Sullivan, M. Reid,M., Marshall, J., Hyland, A., Loree, T., Lillis, C., Hauck, L., Wactawski-Wende, j., Scannapieco, F. Chronic Periodontitis and the Risk of Tongue Cancer. Arch Otolaryngol Head Neck Surg. 2007;133:450-454. http://archotol.ama-assn.org/cgi/content/short/133/5/450 Accessed 4/29/13.
22. Chronic Gum Disease Linked to Risk of Tongue Cancer. May 22, 2007. SUNY News Release. http://www.buffalo.edu/news/8643?print=1 Accessed 4/29/13.
23. Tezal M, Scannapieco FA, Wactawski-Wende J, et al. Local Inflammation and Human Papillomavirus Status of Head and Neck Cancers. Arch Otolaryngol Head Neck Surg. 2012;138(7):669-675. doi:10.1001/archoto.2012.873. http://archive.is/2s7D Accessed 4/29/13.
24. Gillison ML, D'Souza G, Westra W, Sugar E, Xiao W, Begum S, Viscidi R. Distinct risk factor profiles for human papillomavirus type 16-positive and human papillomavirus type 16-negative head and neck cancers. J Natl Cancer Inst. 2008 Mar 19;100(6):407-20. doi: 10.1093/jnci/djn025. Epub 2008 Mar 11. http://jnci.oxfordjournals.org/content/100/6/407.full.pdf+html Accessed 4/30/13.
25. HPV Vaccines. Centers for Disease Control and Prevention. Last Updated 2/15/13. http://www.cdc.gov/hpv/vaccine.html Accessed 4/20/13.
26. Report to the Nation shows U.S. cancer death rates continue to drop; Special feature highlights trends in HPV-associated cancers and HPV vaccination coverage levels. National Cancer Institute Press Release. 1/7/13. http://www.cancer.gov/newscenter/newsfromnci/2013/ReportNation Accessed 4/30/13.
27. Delta Dental Debuts myDentalScore. Delta Dental News Room. March 11, 2013. http://www.deltadental.com/Public/NewsMedia/NewsReleaseMyDentalScore201303.jsp Accessed 4/20/13.
28. DiGangi, P, Gutkowski, S, Seckman, C. Interventionists A change virus. RDH Magazine. http://www.rdhmag.com/articles/print/volume-29/issue-8/feature/interventionists-a-change-virus.html Accessed 4/30/13.
29. Jaslow, R. Oral Sex and throat cancer: Michael Douglas HPV report spotlights "epidemic." CBS News, Reported June 3, 2013. http://www.cbsnews.com/8301-204_162-57587350/oral-sex-and-throat-cancer-michael-douglas-hpv-report-spotlights-epidemic/ Accessed 10/12/13.