You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
INTRODUCTION
It is difficult to believe that preventive dentistry has only been in practice for over one hundred years in the United States. In those 100 years we have seen advances in our delivery of professional oral health care in all disciplines.
However, despite these advances, dental caries remains the most prevalent chronic disease in both children and adults, even though it is largely preventable. Although caries has significantly decreased for most Americans over the past six decades, large disparities remain among some population groups. In addition, this downward trend has recently reversed for young children.1 The statistics have not radically changed since the last version of this course in that dental caries still affects more than 33% of U.S. children aged 2 - 5 years and approximately 50% of children 12 - 15 years old. One fourth of adults aged 65 and older are endentulous.
Oral and oropharyngeal cancers are the largest group of those cancers which fall into the head and neck cancer category. Common names for it include such things as mouth cancer, tongue cancer, tonsil cancer, and throat cancer. Approximately 54,000 people in the U.S. will be newly diagnosed with oral cancer in 2021.2 The preventive topics presented in this course are important for the dental professional to know as they care for their patients.
CARIES RISK ASSESSMENT
Dental caries is defined as a transmissiblelocalized infection caused by a multifactorial etiology. In order for dental caries to develop, four interrelated factors must occur:
1) the patient's (host) diet must consist of repeated digestion of refined carbohydrates;
2) the host's resistance to disease is decreased;
3) the factor of time; and
4) there must be a specific bacteria (Streptococci mutans or S. mutans) present in the dental plaque.
The S. mutansplay an active role in the early stages of the caries process, whereas the bacteria lactobacillicontribute to the progression of the carious lesion. Without bacteria, no caries can develop. Carious lesions must be diagnosed in conjunction with both a clinical examination and imaging to verify suspicious lesions especially interproximal lesions. Light fluorescence may also be used as an adjunct in caries diagnoses.
Enamel is the most highly mineralized hard tissue in the body. The enamel matrix is made up of a protein network consisting of microscopic mineralized hydroxyapatite crystals arranged in rods or prisms. The protein network facilitates the diffusion of fluids, such as calcium and phosphate ions distributing these ions throughout the enamel. As carbohydrates are consumed by the host, the carbohydrates are broken down in the oral cavity by the protein enzyme amylase. This reaction causes lactic acid to be produced, thereby demineralizing the enamel matrix. If the demineralization of enamel is not reversed by the action of fluoride or calcium and phosphate ions, then the demineralization process continues further into the tooth structure, affecting the dentinoenamel junction (DEJ) and eventually the dentinal layer. The term "overt or frank" caries is used when it reaches the DEJ.
A carious lesion develops in three stages of demineralization. The first stage in demineralization of enamel is called the incipient lesion or "white spot" (Figure 1). This beginning carious lesion can be reversed with the daily use of fluoride or calcium and phosphate, persistent oral hygiene care, and a reduction of refined carbohydrates. The second stage involves the progression of demineralization leading to the DEJ and into the dentinal layer. The third stage is the actual cavitation in the dentinal layer. Neither of the last two stages can be reversed and require mechanical removal of dental caries.
There are three levels of preventive dentistry that the dental professional should understand when educating patients in the dental caries process. The first step is primary prevention. This prevents the transmission of S. mutansand delays the establishment of bacteria in infants, toddlers, and young children. The second step is secondary prevention, which prevents, arrests, or reverses the microbial shift before any clinical signs of the disease occur. The third step focuses on limiting or stopping the progression of the caries process by initiating remineralization therapy of existing lesions.
Prevention Step One - Transmission and Establishment of S. Mutans
Specifically, bacteria are transmissible via the parents or other primary caregivers. The most common routes of infection are from close contact with the child and from everyday nursing items, such as baby bottles, pacifiers, and spoons. The colonization of S. mutansis facilitated by a frequent sucrose-rich diet of the parent/caregiver, as well as the child. The higher the count of S. mutanspresent in the primary caregiver's oral cavity, the more risk for the child. Another important factor in the caries process is that the earlier the S. mutansare introduced into the oral cavity and the greater number of bacteria present, the more likely it is that caries will develop in both the primary and permanent dentition. The ‘window of infectivity' of S. mutansis usually between ages 19 months and 31 months. For these reasons education of the parents and primary caregivers is extremely important.
Prevention Step Two - Microbial Shift
Once S. mutansand lactobacillibacteria are established in the oral cavity, the greater the risk for future caries to develop. Where biofilm (plaque) accumulates, the bacterial count is considered to be higher, as in areas in the oral cavity that are difficult to reach during oral hygiene, such as pit and fissures. Newly erupted teeth are deficient in mineral content (calcium and phosphate), making them more susceptible to bacteria. By introducing antimicrobial agents, such as fluoride the bacterial count may be significantly reduced.
Prevention Step Three - Demineralization of Enamel
When refined carbohydrates are introduced into the oral cavity, lactic acid production occurs as an end product of S. mutans, causing the saliva pH to drop from a neutral pH of approximately 7 to an acidic pH of 4.5-5.0. This metabolizing acidogenic bacteria's lactic acid production begins to demineralize the enamel. Common reasons for the prolonged acid conditions include: increased carbohydrate intake, reduced clearance of lactic acid due to low saliva content (hyposalivation or xerostomia), impaired saliva pH buffer capacity, and biofilm accumulation due to insufficient oral hygiene care. The more acidogenic bacteria present, the more lactic acid produced.
When saliva is released into the oral cavity via the salivary glands, the pH of the saliva returns to normal or an approximate pH of 7 and a period of remineralization (repair) occurs. This process is facilitated if fluoride or calcium and phosphate ions are present locally. The balance between demineralization and remineralization is crucial. If the balance is not maintained and demineralization occurs too frequently, then an incipient lesion will occur. This incipient or ‘white spot' lesion may take up to approximately 9 months or more to be seen via digital imaging or radiographically as a radiolucency or dark spot on a bite-wing radiograph.
Carious Lesions Occur in Four General Areas of the Tooth
• Pit and Fissure Caries (Figure 2)
Includes Class I occlusal surfaces of posterior teeth, lingual pits of maxillary incisors, buccal surfaces of mandibular molars.
• Smooth Surface Caries & Interproximal Surface Caries (Figure 3)
Includes Class V buccal, lingual surfaces of anterior and posterior teeth and Class II interproximal surfaces of all teeth below the interproximal contact points.
• Root Surface Caries (Figure 4)
A more common lesion now found clinically, due to patients keeping their teeth longer.
• Secondary or Recurrent Caries (Figure 5)
Includes caries seen adjacent to or beneath an existing restoration.
CAMBRA and CRA
In the 2000's there was a concept shift in the approach of caries prevention. Caries Management by Risk Assessment (CAMBRA) was developed by the California Dental Association in conjunction with the University of California - San Francisco. The science behind CAMBRA and the proof of its success is indisputable.3 The philosophy of CAMBRA is to assess every patient on an individual basis and this model has become the standard of care.3
Caries risk assessment (CRA) defined is to predict future caries developmentbefore the clinical onset of the disease.3 Risk factors are the lifestyle and biochemical determinants that contribute to the development and progression of the disease. Examples of patients who are at risk include those with certain socioeconomic factors (low education level, social deprivation, low income), those with certain factors related to general health (diseases, a physically or mentally compromised individual), and those with epidemiologic factors (living in a high-caries family or having a high past-caries experience). The key to dental caries risk assessment is to assess every patient on an individual basis, determine the possible risk factors and establish an individual treatment plan for each patient.3 These methods include radiographs, a laser tool that measures fluorescence within the tooth, evaluating nutritional habits and saliva flow, and testing levels of acid-producing bacteria.3
Methods to Determine Caries Risk
(Table A)
Each of these categories must be addressed at each dental examination to determine risk assessment, as a patient's oral condition may be different due to physiological changes or self-care practices. A current report should be placed in the patient's chart. Oral instructions at their appointment, as well as written instructions are given to the patient before they leave indicating their home or self-care instructions.7
Newer Detection Technologies
With today's technology, caries detection has become more precise which leads to treatment specific to individual patient's need. The "old ‘drill and fill' … does not address the full disease process, including microbial activity and the balance between enamel remineralization and demineralization".4
This understanding is reflected in the decision of the Code Maintenance Committee of the American Dental Association to approve an insurance code specifically for a "nonionizing diagnostic procedure capable of quantifying, monitoring, and recording changes in structure of enamel, dentin, and cementum".5 The new CDT code, D0600, took effect on January 1, 2017.5
Non-ionizing diagnostic procedures refer to devices used in dentistry to record changes in tooth structures to detect caries before it can be diagnosed clinically or radiographically.6 Some caries detection units feature lasers that cause fluorescence of the mineral structure of the tooth and some use transillumination. Transillumination has been shown to be more sensitive to early demineralization than dental radiography.6
Technology will continue to advance and our ability to address the caries disease issue will improve. It would be easy to just rely on the technology of the tool in hand; however, there is no substitute for research, education and experience. Dave St. Ledger wrote that "there are no short cuts in any diagnosis. Clinical visual, tactile, radiographic, patient dental history and susceptibility all play a role in individualized care. Experience is crucial."6
SKIN, LIP & ORAL CANCER
Introduction
The patient must be screened for oral cancer at the initial appointment and each routine dental examination by performing an extraoral and intraoral examination. Imaging is normally prescribed based on an individual's diagnoses, but suspicious areas in the oral cavity may require additional imaging. There are various types of pathology lesions found in the oral cavity and the head and neck regions. Even though the allied dental professional cannot diagnose lesions, they should be educated in oral pathology to ‘interpret' lesions when assisting the dentist in his or her diagnosis. Four categories are explained in this course. Each dental facility should have oral pathology books and/or online resources with color photographs available for the dental professionals to assist with diagnoses.
Four Types of Pathologies
Candidial Leukoplakia (Chronic Hyperplastic Candidiasis) - "White Lesion"
Etiology - an infection of the oral mucosa caused by fungus; candida albicans or infected epithelial tissue, which becomes hyperplastic with a formation of excess surface keratin (callused).
Typical Visual Cues - a circumscribed white plaque found at the site of fungal infection that will not rub off with gauze, most often found on the anterior buccal mucosa adjacent to the commissure (corner of the mouth); may occasionally be found at the lateral border of the tongue.
Useful Clinical Information - more common in adults, considered a painless and persistent lesion.
Treatment Recommendations - antifungal agents for treatment of oral candidiasis, such as Mycostatin Nystatin, Mycelex clotrimazole, or Fungizone amphotericin B. Systemic antifungal agents for chronic candidiasis include: Nizoral Ketoconazole, Diflucan Fluconazole or Sporanox Itraconazole.
Clinical Significance - oral lesions found in tobacco users should be viewed with increased suspicion for possible pre-cancerous or cancerous lesions. (Figure 6)
Erythroplakia - "Red Lesion"
Etiology - a significant risk factor to the oral mucosa is chronic exposure to carcinogenic components found in all types of tobacco. The other common risk factor is chronic alcohol exposure. Even worse is a combination of both.
Typical Visual Cues - a circumscribed, or ill-defined, erythematous plaque that varies in size, thickness and surface configuration. It has a velvety appearance and occurs most frequently on the floor of the oral cavity, ventral area of the tongue and the soft palate.
Useful Clinical Information - a painless and persistent lesion, found more commonly in adult males and patients who report tobacco exposure.
Treatment Recommendations - the patient should be counseled in a tobacco cessation program if biopsies reveal that the lesion is premalignant. Then, a more extensive therapy is indicated and the patient should be re-evaluated at regular intervals for other oral mucosal changes.
Clinical Significance - erythroplakia occurs less frequently than leukoplakia, but it is much more likely to exhibit microscopic evidence of premaligancy. (Figure 7)
Squamous Cell Carcinoma
Etiology - idiopathic (unknown). Risk factors include: tobacco use, alcohol use, sun radiation, genetic predisposition, nutritional deficiency, immunosuppression, and infections, such as candidal leukoplakia and human papillomavirus.
Typical Visual Cues - a deep-seated ulcerated mass, fungating ulcerated mass, ulcer margins commonly elevated, adjacent tissues commonly firm to palpation, and may have residual leukoplakia and/or erythroplakia.
Useful Clinical Information - more common in adult males, continuous enlargement, local pain, referred pain often to the ear, and paresthesia often of the lower lip.
Treatment Recommendations - patient should be counseled to stop tobacco use and given a referral to a local medical treatment facility for appropriate treatment (surgery, radiation therapy, chemotherapy), and a careful periodic re-evaluation.
Clinical Significance- early diagnosis is essential for cure, presence of lymph node metastasis greatly worsens the prognosis, approximately 50% of patients have evidence of lymph node metastasis at time of diagnosis (that is why the extraoral examination is so critical at the time of each intraoral examination), and patients who have had one cancer are at greater risk of having a second oral cancer. The overall 5-year survival rate is 45-50%. (Figure 8)
Malignant Melanoma
Etiology - a malignant neoplasm of melanin-producing cells. Chronic exposure to sun radiation and a fair complexion increases the risk for skin lesions.
Typical Visual Cues - larger than 0.5 cm in diameter, irregular margins, irregular pigmentation, any change in pigmentation, ulceration of the overlying mucosa, macular (superficial spreading) or elevated (nodular), and most often occurs on gingiva and the palate.
Useful Clinical Information - occurs most often in adult males, usually painless, rapidly enlarging.
Treatment Recommendations - refer to a local medical treatment facility for the appropriate surgery and chemotherapy.
Clinical Significance - malignant melanoma is an extremely aggressive form of cancer, early diagnosis is essential for cure, patients with oral mucosal lesions generally have a poor prognosis. For skin, the 5-year survival rate is 65%and for oral the rate is 20%. (Figure 9)
Oral Management for the Cancer Patient
Bacterial Plaque Control
Start oral hygiene instruction at first appointment and emphasize preventive infection control procedures and potential oral side effects associated with cancer therapy. Toothbrushing instructions include using a soft or extrasoft toothbrush; a flavored dentifrice may not be tolerated, but fluoride is essential. Mouthrinses include saline solution to moisten the mucosa or baking soda rinses for managing oral mucositis. Chlorhexidine gluconate rinsing may also be recommended for antibacterial properties. Commercial mouthrinses that contain alcohol should be avoided.
Daily Fluoride Therapy
Daily fluoride therapy is indicated for patients about to undergo head and neck radiation therapy, if the salivary glands are in the field of radiation. Make impressions and fabricate a custom fluoride tray, advise the patient to apply custom trays lined with prescription neutral sodium fluoride gel to the teeth for four minutes once daily or use brush-on sodium fluoride varnish. Advise patient to refrain from eating, drinking, or rinsing for 30 minutes following fluoride application.
Dietary Instructions
Instruct the patient in the preparation of foods. Avoid highly cariogenic foods such as carbohydrates and also spicy foods. A soft, bland diet is recommended. Water is recommended throughout the day to moisten the oral cavity. Saliva substitutes are also recommended to decrease the risk of caries.
Avoid Alcohol and Tobacco Products
If the patient uses tobacco products, a logical step for the cancer patient is to start tobacco cessation counseling. See the ADAA continuing education course on tobacco cessation for further recommendations.
ORAL HYGIENE EDUCATION
The Development of Dental Plaque
Plaque is a biofilm that contributes to two oral diseases: dental caries and periodontal disease. It is a complex community of microorganisms that have a negative surface charge that attaches to the host surface enamel or gingiva. Biofilm can also contribute to peri-implantitis. The initial layer or formation of plaque is called the acquired pellicle.This layer will reform within two hours after removal and will also form on artificial prosthesis, such as dentures. With over 700 species of aerobic and anaerobic bacteria in the human oral cavity, microbes grow as complex colonies in biofilm. In fact, it takes only two days for plaque to double in mass. Plaque requires the following to metabolize: streptococci mutansand a processed carbohydrate. The end product, lactic acid consists of intracellular polysaccharides and extracellular polysaccharides. When plaque is not removed from the oral cavity it may mineralize and become calculus. This mineralized formation is formed by calcium and phosphates in the saliva and it has been found that tobacco use accelerates the formation of calculus. However, recent research studies link plaque as the contributing factor to periodontal disease rather than calculus. Daily removal of biofilm is critical to reduce oral diseases.
Manual versus Powered Toothbrushes
Both manual and power toothbrushes can effectively remove plaque if patients use correct technique and brush for an adequate time period. (Figures 10, 11) Certain toothbrush designs, however, provide more effective removal than others. Some studies show oscillating-rotating power brushes can be more effective at plaque removal than manual brushes. Power toothbrushes were shown to be as safe to use as manual toothbrushes if used properly.
There are several manual toothbrushing techniques. They include the horizontal scrub, Bass, Stillman, Charters, and Fones, to name a few. The most popular method that an uneducated patient uses is the horizontal scrub. Unfortunately, gingival and enamel damage can occur with aggressive strokes and too firm of bristles. The Stillman method is used for massage and stimulation of the gingiva with a 45 degree angle of the bristles and a vibratory/pulsing method. The Charter method also involves a 45 degree angle with the bristles and a rotary or vibratory motion forcing the bristles interproximally. The Charter's method can be recommended for orthodontic patients to clean ortho brackets and bands.
A preferred method for adults is the Modified Bass Method. (Figure 12) This method was the first to focus on the removal of plaque and debris from the gingival sulcus with the combined use of the soft toothbrush and dental floss. The method is effective for removing plaque at the gingival margins and controlling plaque that leads to periodontal disease and caries. In the Bass technique, the toothbrush is positioned in the gingival sulcus at a 45-degree angle to the tooth apices. A vibratory action, described as a back-and-forth horizontal jiggle, causes a pulsing of the bristles to clean the sulcus. The term ‘modified' indicates a final ‘sweep' with the toothbrush toward the occlusal surfaces to remove debris subgingivally. Ten strokes are recommended for each area. This is the only toothbrush method that places the toothbrush bristles into the sulcus.
For children, the rotary method called the Fones technique (Figure 13) is preferred since children do not have the manual dexterity for a more advanced technique. The Fones technique is a circular method similar to the motion of the old rotary telephone. The teeth are clinched and the toothbrush is placed inside the cheeks. The toothbrush is moved in a circular method over both the maxillary and mandibular teeth. In the anterior region, the teeth are placed in an edge-to-edge position and the circular motion is continued. Children adapt to this technique rather quickly.
There are many powered toothbrushes available on the market. There are also less expensive battery-powered toothbrushes available for patients to try. Studies have shown powered toothbrushes are an excellent tool for all patients, particularly those with low manual dexterity or physical limitations. The larger handle is ideal for patients who cannot grip the smaller manual toothbrush handles, such as patients with arthritis or stroke victims. The patient should be encouraged to try both manual and powered toothbrushes and determine which is best for them. However, the patient should be instructed to use the new toothbrush for at least four weeks. It takes approximately 30 days for someone to develop a habit. Trying new dental products requires time to adapt to new habits.
Whichever toothbrush is used, the patient should be taught to remove plaque in a sequential order when brushing to make sure they don't skip any surface areas of the enamel or exposed cementum. The patient should be shown in the mirror the proper technique and their instruction should also include brushing their tongue to remove debris and bacteria. The patient should show that they understand their oral hygiene instruction by demonstrating it back to the dental professional. A combination of oral and written instructions is always preferred. Studies have shown that too much instruction at one time is overwhelming for the patient and they will not adopt new habits unless they understand and believe that they have value and are important.
Auxiliary Aids
Dental Floss and Flossing Methods
There are many different types of floss or tape on the market: waxed vs. unwaxed, mint vs. cinnamon or bubblegum, floss vs. floss holders or floss threaders. Many patients will ask: "Is waxed floss or unwaxed floss better?" The answer should be simply, "I'm glad you're flossing. It's whatever you prefer." Some studies indicate that waxed floss is preferred because it gets through the contact points easier. Other studies indicate that dental professionals are concerned with the amount of wax that may accumulate in the gingival sulcus.
Another question patients ask frequently is, "Do I floss before or after brushing?" Again, it doesn't matter. As long as they are flossing properly, dental professionals are thrilled. The point of brushing and flossing is plaque removal. By removing the irritant plaque and reducing the bacterial count in the saliva, the patient is making a significant difference in preventing caries and periodontal disease.
There are two flossing methods available to teach your patients. One is the circle or loop method and the other is the spool method. The circle or loop method is preferred for children or any patient with low manual dexterity. A piece of floss approximately 18 inches long is tied at the ends to form a loop or circle. The patient uses the thumb and index finger of each hand in various combinations to guide the floss interproximally through the contacts. When inserting floss, it is gently eased between the teeth with a seesaw motion at the contact point, making sure not to snap the floss and cause trauma to the gingival papilla. Once through the contact area, gently slide the floss up and down the mesial and distal marginal ridges in a C-shape around the tooth directing the floss subgingivally to remove the debris.
The spool method (Figures 14A, 14B, 14C) utilizes a piece of floss approximately 18-24 inches long where the majority of the floss is loosely wound around the middle finger of one hand and a small amount of floss around the middle finger of the opposite hand. The same procedure is followed as the loop method when positioning the floss interproximally. After each marginal ridge is cleaned, the used floss is moved or spooled to the other hand until all supragingival and subgingival areas have been cleaned, including the distal areas of the posterior teeth.
Patients with fixed prosthesis such as bridges, orthodontics, and bonded orthodontic retainers should be encouraged to use floss threaders (Figures 15, 16) to remove debris. The floss is threaded underneath the prosthetic to remove any debris caught underneath. Patients should be instructed on their use and again asked to demonstrate to the dental professional that they understand and know how to use it.
Floss holders (Figure 17) are an alternative if the patient has difficulty flossing manually or for a patient with large hands, physical limitations, a strong gag reflex, or low motivation for traditional flossing. A floss holder is a good alternative to not flossing at all and should be shown to patients as a means of removing plaque.
Toothpicks or Wooden/Plastic Triangular Sticks
If your patients have large diastemas or food impaction areas, they should be encouraged to utilize interproximal sticks such as Stim-U-Dents®. Made of balsa wood, Stim-U-Dents® are used to remove debris and plaque, and are preferred by dental professionals over standard toothpicks because toothpicks can splinter into the gingiva and damage the gingival tissue. If patients do not have access to floss, they can use the wooden balsa sticks to remove plaque and stimulate the gingiva. (Figure 18)
Interproximal and Uni-tufted Brushes
These small interproximal brushes are attached to handles and are used for large spaced interproximal areas and for orthodontic patients to use between their brackets to remove debris. There are a variety of brushes available, including travel sizes for pockets and purses. The brushes are tapered for easy access to difficult areas and patients seem to adapt well to instructional use. (Figure 19)
FLUORIDES
Introduction
Both community water fluoridation, known as systemic or pre-eruptive fluoride and topical fluoridation, also known as post-eruptive fluoride, have proven to be an important mechanism in preventing dental caries in the United States since the 1950's. Through studies, researchers have discovered that not only has water fluoridation contributed to the decline in dental caries, but also the post-eruptive effect of fluoride has played an even more vital role in reducing dental caries.
Current Theories Regarding Fluoride Use
The current theory is that a daily use of fluoride-containing dentifrices has significantly reduced the dental caries level in the United States. Other sources of fluoride include: added fluoride to city water sources; naturally occurring water fluoride in well water; fluoridated dentifrices (toothpastes); over-the-counter mouthrinses; processed food and beverages at manufacturing plants that utilize fluoridated city water; prescription rinses, gels, pastes, and tablets; professional fluoride varnish applications; and both in-office and at-home topical fluorides. This consistent application of fluoride to enamel has reduced dental caries and has significantly changed how dentistry is practiced today.
By current convention, many dental professionals administer professional topical fluoride treatments to patients at their preventive maintenance appointments. However, is this routine procedure necessary for every patient? Although concentrated topical fluoride treatments usually are intended for annual or semiannual prophylaxis visits, a decline in caries prevalence brings into question the continuing need for such treatment in individuals who are caries-free, at a low caries risk, use fluoridated toothpaste, and ingest fluoridated water. The decision to use a professionally applied topical fluoride should be based on a recent clinical examination, as well as scientific evidence.
Since current practice is to deliver a topical fluoride system to every young patient, the dental profession is faced with an ethical quandary when dealing with this issue. If a patient does not show evidence of active caries, should the patient be given a professional fluoride treatment at the prophylaxis appointment? With exposure to so many outside sources, the patient may be receiving adequate amounts of fluoride to maintain a caries-free condition without routinely scheduled professional fluoride applications. These frequent exposures to low concentrations of fluoride, as received from toothpastes, are more effective in the prevention of caries than infrequent exposures to high concentrations of fluoride, as received from professional treatments. The American Dental Association (ADA) utilizes evidence-based research when making clinical recommendations. The ADA states that "patients whose caries risk is lower may not receive additional benefit from professional topical fluoride." Recommendations to use topical fluoride applications on your patient should be determined by whether or not the patient is exposed to multiple sources of fluoride or has other caries risk factors.
Pre-eruptive vs. Post-eruptive Fluoride
At the time of tooth eruption, enamel is not quite completely mineralized and will undergo what is now called the post-eruptiveperiod (formally known as the topical effect) that will take approximately two years. Throughout this enamel maturation period, fluoride continues to accumulate in the outer surfaces of the enamel. This fluoride is derived from the saliva, as well as exposure to fluoride-containing products such as food and beverages. Most of the fluoride incorporated into the developing enamel occurs during what is now called the pre-eruptive(formally known as the systemic effect) period of enamel formation, but also occurs topically during the post-eruptiveperiod of enamel maturation.
Types of Professional Fluoride
The most widely used types of fluoride by dental professionals to prevent or reduce caries are a neutral sodium fluoride (NaF) and acidulated phosphate fluoride (APF). Sodium fluoride forms calcium fluoride in enamel after use. It is also recommended for patients with porcelain and ceramic restorations because of its non-etching property. Though some practices still use disposable trays for delivering fluoride applications, the now preferred method is sodium fluoride varnish.7 This is supported by both the ADA and the AAPC.8, 9 It is easy to use in any setting (making it great for mission trips), has a higher ppm (parts per million) of fluoride and well tolerated by patients young and old.
One Minute vs. Four Minute Fluoride Applications
Research studies continue to show that fluoride uptake in enamel is time-dependent due to a diffusion-controlled process and that it should be left on the teeth for the full four minutes. Although the most uptake of fluoride is in the first minute, research shows that the full 4 minutes provides the best topical benefit. The ADA states "there are considerable data on caries reduction for professionally applied topical fluoride gel treatments of 4 minutes or more. In contrast, there is laboratory, but no clinical equivalency data on the effectiveness of 1-minute fluoride gel applications".10 Because an early study reported that fluoride uptake by dental enamel increased in an acidic environment, fluoride gel is often formulated to be highly acidic (pH of approximately 3.0).7
Fluoride Varnish
Most varnishes contain 5% sodium fluoride with only .3-.5 ml of the varnish being applied. Patient compliance, especially with small children appears to be better than with professional fluoride tray applications. The application includes starting with clean tooth surfaces and painting the varnish on the teeth (Figure 20), after drying the tooth surface. The varnish should be left on the tooth surface until the next day, as the fluoride continues to be released into the enamel. The patient should be instructed not to brush until the next morning. Always follow manufacturer's recommendations. Based on caries risk, the fluoride varnish recommendations include reapplying at 4 to 6 month intervals. Fluoride varnish is an important dental therapy for high-risk patients.
The application of fluoride varnish is not intended to adhere permanently; this method holds a high concentration of fluoride in a small amount of material in close contact with the teeth for several hours.10 This underscores the need to fully assess the individual to determine which treatment option is best for that patient.
The current guidelines from the ADA Evidence-based Topical fluoride Guide11: (Table B)
The American Dental Association (ADA) has a policy to update clinical recommendations and evidence every five years. Their next update is due 2018 - 2019.10 This course reflects the current guidelines as presented.
Additional Notes
The ADA recommends that for patients with active and rampant caries topical fluoride applications should be done more frequently. Note that a professional prophylaxis is not needed prior to the application of any professional topical fluoride product because fluoride uptake and caries inhibition are not improved by a prophylaxis.10 Also, the use of a fluoride prophylaxis paste does not replace a professionally applied fluoride application.
Besides receiving topical fluoride treatment on a quarterly basis, the patient with rampant caries will require a home prescriptive fluoride-treatment program as well. Patients with active caries require professionally applied fluoride applications at least twice a year. Based on a recent clinical examination, if a patient ingests sufficient fluoridated water and is caries free, a topical fluoride treatment is not necessary. There is little fluoride deposition lasting more than 24 hours when fluoride is applied to sound, fully maturated enamel. Therefore, there appears to be no preventive benefits from the application of fluoride to adult patients with sound enamel.10
Root Surface Caries on the Rise
Root surface caries has increased due to the increased retention of teeth during adulthood thanks to various caries-preventive measures and patients living longer. About one-half of U.S. adults are affected with root surface caries by age 50, with an average of about three lesions by age 70. Fluoride is very effective in preventing root surface caries.
Amorphous Calcium Phosphate (ACP)
ACP has anticariogenic properties to promote the remineralization of enamel and cementum, as well as balancing the pH of saliva and reducing dentinal sensitivity. Regular application of ACP with fluoride increases levels of calcium and phosphate levels in biofilm and tooth structure. In fact, an addition of 2% ACP (i.e. Recaldent™) to as little as 450 ppm fluoride can significantly increase the incorporation of fluoride ions into biofilm and co-localize calcium and phosphate ions with fluoride ions at the tooth surface. An adjunct treatment of ACP and a 1,100 ppm fluoridated dentifrice (toothpaste) can decrease bacteria and increase mineralization. Patients who benefit from ACP include conditions such as orthodontic, white spots, polypharmacy, tooth whitening, oncology, hypersensitivity, high caries risk, xerostomia, and
acid erosion due to sodas and other drinks.
DIET AND DENTAL CARIES
Introduction
A number of studies have shown a clear relationship between fermentable carbohydrate consumption and dental caries. The amount of sugar in the diet is not as important in caries progression as the frequency and form of consumption. For example, foods such as raisins, processed starches (i.e. pies, cakes, cookies) and candies that adhere to the teeth for some time will continue to slowly release sugar. The local bacteria (S. mutans) use carbohydrates and extends the decrease in the plaque pH. Similarly, any food or beverage that contains fermentable carbohydrates and is consumed over a prolonged period or with increased frequency will have the same effect.
Fruits in general tend to have low cariogenic potential, with the exception of dried fruits and certain fresh fruits. Apples, bananas, and grapes contain 10-15% sucrose, citrus fruit 8%, and berries and pears only 2%. Although citrus fruits are high in water, stimulate saliva production, and provide an excellent source of vitamin C, they can potentially erode tooth enamel if consumed in large quantities over an extended period of time.
Non- or Low-Acidogenic Foods
• Raw vegetables, such as broccoli, cucumber, lettuce, carrots, peppers.
• Meat, fish, poultry.
• Beans, peas, nuts, natural peanut butter.
• Milk, cheeses, flavored yogurts.
• Corn chips, peanuts, popcorn.
• Fats, oils, butter, margarine.
• Non-sugar sweeteners, such as xylitol®, nutrasweet®, aspartame®, saccharin®, sucralose®.
Soft drinks, sport drinks, and energy drinks containing sugar are big business in the United States. Frequent consumption of sugary drinks has long been known to contribute to dental caries. According to the Centers for Disease Control (CDC), consumption of soft drinks in the United States has increased over the last 30 years with both adults and children. Soft drinks have been linked to obesity and type 2 diabetes. Teenagers and young adults consume more sugar drinks than other age groups. Males consume more soft drinks than females and low-income Americans consume more soft drinks than those with higher incomes.
A non-diet soft drink is made from carbonated water, added sugar and flavors. Each can of soda contains the equivalent of about ten teaspoons, or 40 grams, of sugar. Mountain Dew® is so popular in the United States that the coined phrase "Mountain Dew Mouth" is a recognized term used by the dental profession for patients diagnosed with rampant caries and/or erosion.
PIT & FISSURE SEALANTS
Introduction
Sealants have been endorsed by the American Dental Association (ADA) and the United States Public Health Service as being effective in preventing pit and fissure caries. Pit and fissure caries accounts for over 80% of active caries in children; however, these surfaces make up only 15% of the total tooth surfaces. Sealants must not be overlooked as another form of preventive dentistry, along with plaque control, fluoride therapy and sugar discipline.
The ADA states that sealants are "broken into two categories based on the reaction that takes place as they set in the mouth. Glass ionomers undergo an acid-base reaction as they set, while composite resins set through a polymerization reaction that is usually initiated by a dental curing light. Resin-modified glass ionomers and polyacid-modified resins set by a combination of these two reactions, resulting in sealant products with differing characteristics that vary"12 (widely).
The Criteria for Selecting Teeth for Sealants
The criteria for selecting teeth for sealant placement are a deep occlusal fissure, fossa (Figure 21) or incisal lingual pit. A sealant may be contraindicated if:
1) a patient's behavior does not permit the required dry-field to place sealants,
2) an open carious lesion exists,
3) caries exist on other surfaces of the same tooth and restoration will disrupt an intact sealant,
4) a large occlusal restoration is already present.
The disease susceptibility of the tooth should be considered when selecting teeth for sealants, not the age of the patient. Sealants appear to be equally retained on occlusal surfaces of both primary and permanent dentition. Sealants should be placed on the teeth of adult patients if there is evidence of existing or impending caries susceptibility, such as a diet excessive in carbohydrates or as a result of a drug or radiation-induced xerostomia.
Types of Sealant Materials
There are two types of resin-based sealants available today, filled and unfilled. Filled sealants are a combination of resins, chemicals and fillers. The purpose of the filler is to increase bonding strength and resistance to abrasion and wear. Due to the hardness and wear resistance of filled sealants, they must be checked after placement with articulating paper and adjusted with a dental handpiece and appropriate bur. Unfilled sealants have a higher ratio of resin to filler material, and do not need to be adjusted with a dental handpiece; they are in essence self-occluding. Due to high viscosity (rate of flow) of unfilled sealants, they readily flow into the pits and fissures.
Because fluoride uptake increases the enamel's resistance to caries, the use of a fluoridated resin-based sealant may provide an additional anticariogenic effect. Fluoride-releasing sealants have shown antibacterial properties, as well as a greater artificial caries resistance compared to a non-fluoridated sealant material. The fluoride will leach out over a period of time into the adjacent enamel. Eventually the fluoride content of the sealant should be exhausted, but the content of the enamel greatly increased.
Retention Keys
For sealant retention the surface of the tooth must:
1) have a maximum surface area,
2) have deep, irregular pits & fissures for better retention,
3) be clean, and most crucial to retention
4) be absolutely dry and uncontaminated with saliva residue at the time of the sealant placement.
All of these criteria must be present for a sealant to be retained. If within a few months the sealants are lost, it is most likely due to faulty technique by the clinician.
The Pit & Fissure Sealant Procedure
It is highly recommended that sealant application be performed as a two-person procedure. Even when the patient is an adult, isolation and application are difficult with just one clinician.
1) Prior to the application of a tooth conditioner, the tooth surface should be cleaned by air polishing, polishing with non-fluoridated pumice paste, hydrogen peroxide, or enameloplasty. All heavy stains, deposits, debris and plaque should be removed. After cleaning the occlusal surface, dry the area thoroughly for 10 seconds.
2) Increasing the surface area requires tooth conditioner/etchant, composed of 30%-50% concentration of phosphoric acid. Since sealants do not directly bond to the teeth, the adhesive force must be improved by tooth conditioner. If any of the tooth surfaces do not receive the tooth conditioner, the sealant will not be retained. Application usually includes a small sponge applicator or cotton pellet held with cotton pliers. Isolation of the teeth includes cotton rolls, dry-angles, or ideally with a dental dam. Follow manufacturer recommendations for time. Rinse for 10 seconds. The appearance of the enamel by the tooth conditioner is white, dull and chalky. If the enamel does not appear white and chalky, tooth conditioner is reapplied according to manufacturer instructions. Dry thoroughly before sealant application.
3) The application of the sealant material requires the pits and fissures to be filled and the material brought to a knife-edge approximately halfway-up the inclined plane of the cusp ridge (Figure 22). Any bubbles must be broken before polymerization to prevent a defect. Polymerize with a curing light. Follow manufacturer directions for time.
4) Check the sealant with an explorer for proper placement and polymerization. Check occlusion with articulating paper and check interproximal contacts with floss. If sealant material is present interproximal, use a scaler to remove excess. If occlusion is high, use a slow-speed rotary bur such as a no. 4 round or no. 8 round bur. Recheck the occlusion again. Sealants should be checked at each annual dental examination for retention.
MOUTHGUARDS & SPORTS DENTISTRY
Introduction
Whether for exercise, competition or the simple enjoyment of recreational activity, increasing numbers of health-conscious Americans are involved in sporting activities. Approximately 30 million children participate in various sports programs and another 80 million are involved in unsupervised recreational sports. Dentistry plays a large role in treating oral and craniofacial injuries resulting from sporting activities.
To that end, April has been designated as National Facial Protection Month. Five dental organizations have teamed up to educate the public about preventing sports-related injuries to the head and face by using safety equipment. The Academy for Sports Dentistry (ASD), the American Academy of Pediatric Dentistry (AAPD), the American Association of Oral and Maxillofacial Surgeons (AAOMS), the American Association of Orthodontists (AAO) and the American Dental Association (ADA) are co-sponsoring the annual campaign that encourages parents, caregivers and coaches to help prevent traumatic dental injuries (TDI) in athletes.13 Key to protection are mouth guards and helmets to avoid being sidelined by an injury. The 2018 slogan read:: "…As you suit up for outdoor activities this spring, don't forget to protect your face and head."13
Statistics
More than 5 million teeth are knocked out each year; many during sports activities, resulting in nearly $500 million spent on replacing these teeth each year. In an issue of Dental Traumatologyit was reported among children ages 13-17, sports-related activities were associated with the highest number of dental injuries. Males are traumatized twice as often as females, with the maxillary central incisor being the most commonly injured tooth. Studies of orofacial injuries published over the last twenty years reflects various injury rates dependent on the sample size, the age of participants, and the specific sports. In soccer, where rules are not uniform on wearing mouthguards, only a small percentage of the participants wear them. In baseball and softball, again only 7% wear mouthguards.The National Federation of State High School Association (NFHS) recently stated that of all injuries less than 1% are oral injuries because football players are wearing properly fitted mouthguards. Prior to the use of mouthguards, injuries to the orofacial areas occurred over 50% of the time. The NFHS recommends mouthguards for any sports where there is a potential for orofacial injury from body contact. It is clear that the need for studies, education, and regulations for mouthguard implementation is a major concern in the dental field.
All athletes constitute a population that is extremely susceptible to dental trauma. Dental injuries are the most common type of orofacial injury. An athlete has a 10% chance of receiving an orofacial injury every season of play. It is estimated that mouthguards prevent between 100,000 and 200,000 oral injuries per year in professional football alone. The American Academy of Pediatric Dentistry and the American Dental Association recommend a mouthguard for all children and youth participating in any organized sports activities.
Following is a list of types of injuries an athlete may sustain that are of particular concern to the dental professional.
Soft Tissue Injuries
The face is often the most exposed part of the body in athletic competition and injuries to the soft tissues of the face are frequent. Abrasions, contusions, and lacerations are common and should be evaluated to rule out fractures or other significant underlying injury. These usually occur over a bony prominence of the facial skeleton such as the brow, cheek, and chin. Lip lacerations are also common.
Fractures
Fractures of the facial bones present an even more complex problem. One of the most frequent sites of bony injury is the zygoma (cheekbone). Fractures of the zygoma, occurring as a result of direct blunt trauma from a fall, elbow or fist, account for approximately 10% of the maxillofacial fractures seen in sports injuries. Like the zygoma, the prominent shape and projection of the mandible cause it to be frequently traumatized. Approximately 10% of maxillofacial fractures resulting from sporting activities occur in the mandible when the athlete strikes a hard surface, another player or equipment. In a mandibular fracture, airway management is the most important aspect of immediate care. In both children and adults, the condyle is the most vulnerable part of the mandible. Fractures in this region have the potential for long-term facial deformity. Recent data suggest that condylar fractures in children can alter growth of the lower face.
TMJ Injuries
Most blows to the mandible do not result in fractures, yet significant force can be transmitted to the temporomandibular disc and supporting structures that may result in permanent injury. In both mild and severe trauma, the condyle can be forced posteriorly to the extent that the retrodiscal tissue is compressed. Inflammation and edema can result, forcing the mandibular condyle forward and down in acute malocclusion. Occasionally this trauma will cause intracapsular bleeding, which could lead to ankylosis of the joint.
Tooth Intrusion
Tooth intrusion occurs when the tooth has been driven into the alveolar process due to an axially directed impact. This is the most severe form of displacement injury. Pulpal necrosis occurs in 96% of intrusive displacements and is more likely to occur in teeth with fully formed roots. Immature root development will usually mean spontaneous re-eruption. Mature root development will require repositioning and splinting or orthodontic extrusion.
Crown and Root Fractures
Crown fractures are the most common injury to the permanent dentition and may present in several different ways. The simplest form is crown infraction. This is a crazing of enamel without loss of tooth structure. It requires no treatment except adequate testing of pulpal vitality. Fractures extending into the dentin are usually very sensitive to temperature and other stimuli. The most severe crown fracture results in the pulp being fully exposed and contaminated in a closed apex tooth or a horizontal impact may result in a root fracture. The chief clinical sign of root fracture is mobility. Radiographic evaluation and examination of adjacent teeth must be performed to determine the location and severity of the fracture as well as the possibility of associated alveolar fracture. Treatment is determined by the level of injury.
Avulsion
Certainly one of the most dramatic sports-related dental injuries is the complete avulsion of a tooth. Two to sixteen percent of all injuries involving the mouth result in an avulsed tooth. A tooth that is completely displaced from the socket may be replaced with varying degrees of success depending, for the most part, on the length of time it is outside the tooth socket. If the periodontal fibers attached to the root surface have not been damaged by rough handling, an avulsed tooth may have a good chance of recovering full function. After two hours, the chance for success is greatly diminished. The fibers become necrotic and the replaced tooth will undergo resorption and ultimately be lost. See the American Academy of Pediatric Dentistry website relating to avulsed teeth recommendations for dental professionals called the Decision Tree for the Management of an Avulsed Permanent Tooth.
Emergency Treatment
Due to the high incidence of sports-related dental injuries, it is vital that primary healthcare providers such as school nurses, athletic trainers, team physicians and emergency personnel are trained in the assessment and management of dental injuries. Interested dental professionals can assist these providers by offering to speak at schools or community functions, so that the primary health care providers who will deliver immediate treatment at sporting events understand the proper protocol for orofacial injuries, such as displaced teeth, avulsed teeth, lacerations and crown fractures. The ADA has urged its members to work together with schools, colleges, athletic trainers and coaches to develop mouthguard programs and guidelines to prevent sports injuries.
The main method for preventing orofacial injuries in sports is to wear mouthguards and headgear, consisting of a helmet and face protector. Parental perceptions of children's risks to injury, expenses associated with protective gear, and peer pressure may influence use of mouthguards. The observed patterns of mouthguards wearing by males and females can represent cultural differences, peer pressure, and/or nature of sports played, including the following:
• perceptions that females are less aggressive and thus, a reduced risk of injury may exist,
• perceptions regarding the absence of long-term commitment to a sport may result in a differential willingness to devote resources to females,
• aesthetic appeal may influence protective orofacial gear usage, and
• females may play in non-league-based sports with fewer or less stringent rules or may play less combative sports than males.
The literature indicates the behavior of athletes is most influenced by their coaches. Coaches report that most information about mouthguards comes from sales representatives, educational materials and dentists.
The Ideal Mouthguard
When considering recommendations, an ideal mouthguard:
• protects the teeth, soft tissue, bone structure, and temporomandibular joints
• diminishes the incidence of concussions and neck injuries
• exhibits protective properties that include high power absorption and power distribution throughout the expansion
• provides a high degree of comfort and fit to the maxillary arch
• remains securely and safely in place during action
• allows speaking and does not limit breathing
• is durable, resilient, tear resistant, odorless, and tasteless
The American Society for Testing and Materials and the manufacturers of mouthguards have classified the mouthguards into three types:
Stock Mouthguards
Stock mouthguards may be purchased from a sporting goods store or pharmacy. They are made of rubber, polyvinyl chloride or a polyvinyl acetate copolymer. The advantage is that this mouthguard is relatively inexpensive, but the disadvantages far outweigh the advantages. They are available only in limited sizes, do not fit very well, inhibit speech and breathing and require the jaws to be closed to hold the mouthguard in place. Because the stock mouthguards do not fit well, the player may not wear the mouthguard due to discomfort and irritation. The Academy of Sports Dentistry has stated that the stock mouthguard is unacceptable as an orofacial protective device.
Mouth-Formed Protectors
There are two types of mouth-formed protectors: the shell-liner and the thermoplastic mouthguard. The shell-liner type is made of a preformed shell with a liner of plastic acrylic or silicone rubber. The lining material is placed in the player's mouth, molds to the teeth and then is allowed to set. The preformed thermoplastic lining (also known as "boil and bite") is immersed in boiling water for 10 to 45 seconds, transferred to cold water and then adapted to the teeth. This mouthguard seems to be the most popular of the three types and is used by more than 90% of the athletic population. (Figure 23)
Custom Made Mouth Protectors
This is the superior of the three types and the most expensive to the athlete. But isn't it worth the cost to protect an athlete's teeth from injury? Most parents will spend quite a bit of money on athletic shoes, but might not think about protecting their child's teeth. This mouthguard is made of thermoplastic polymer and fabricated over a model of the athlete's dentition (Figure 24). The mouthguard is made by the dentist and fits exactly to the athlete's mouth. The advantages include: fit, ease of speech, comfort and retention. By wearing a protective mouthguard, the incidence of a concussion by a blow to the jaw is significantly reduced because the condyle is separated from the base of the skull by placing the mandible in a forward position.
Dental Team's Role
Sports dentistry should encompass much more than mouthguard fabrication and the treatment
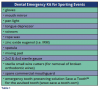
of fractured teeth. As dental professionals, we have a responsibility to educate ourselves and the community regarding the issues related to sports dentistry and specifically to the prevention of sports-related oral and maxillofacial trauma. The American Dental Association (www.ada.org) publishes brochures that explains the different types of mouthguards and their advantages. A field emergency kit is a simple and inexpensive item for the dentist attending a sporting event (see Table 1).
"Fitting mouthguards is a perfect activity for a dental society," says Robert Morrow, D.D.S., Professor of Prosthodontics, University of Texas-San Antonio Dental School. "You simply get a group of dentists together at the school and begin making impressions. It spreads out the costs and cuts down on the time. And it's wo